This is how the AI article summary could look. Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat.
Acute Pancreatitis: Causes, Symptoms, Treatment
Key Points
- Pancreatitis is the inflammation of the pancreas, an organ located behind the stomach. It can be acute (short-term) or chronic (long-term).
-
Acute pancreatitis is a potentially life-threatening condition requiring prompt diagnosis and treatment. It is usually of rapid onset.
-
Abdominal pain (typically in the epigastrium), vomiting and fever are common presenting symptoms.
-
Early recognition and management of severe cases are crucial to improve outcome.
-
Gallstones and excessive alcohol consumption are the most common causes.
1. Definition
- Acute pancreatitis is a rapid inflammation of the pancreas, causing abdominal pain and potentially life-threatening complications. The condition can range from mild to severe.
-
Mild acute pancreatitis: No organ dysfunction or local complications.
-
Moderate acute pancreatitis: Transient organ dysfunction or local complications.
-
Severe acute pancreatitis: Persistent organ dysfunction or severe local complications.
2. Epidemiology
-
Approximately 4,800 hospital admissions occur annually in the UK.
-
Incidence: 50-80 per 100,000 population per year.
-
Mortality rate: 5-10%.
3. Risk Factors
-
Age: Peak incidence between 45-55 years.
-
Sex: Slightly more common in men.
-
Ethnicity: Higher incidence in African Americans.
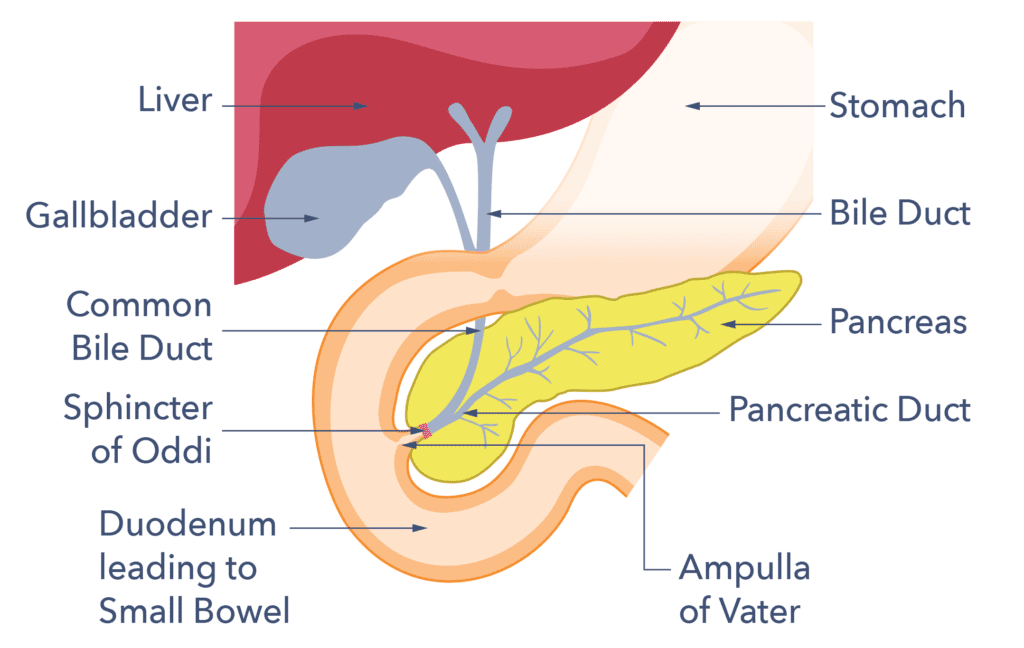
4. Causes
-
Gallstones (45%): Most common cause in the UK.
-
Alcohol (20-30%): More common in men.
-
Drugs: Steroids, azathioprine, and valproate.
-
Infections: Viral (e.g. mumps) and bacterial.
-
Trauma: Abdominal injury.
-
Metabolic disorders: Hypertriglyceridaemia.
-
Genetic disorders: Hereditary pancreatitis.
-
Idiopathic: No identifiable cause.
5. Symptoms
-
Severe, persistent abdominal pain – typically in the epigastrium, and of rapid onset (making a perforated abdominal viscus an important differential diagnosis)
-
Nausea and vomiting.
-
Fever.
-
Abdominal tenderness.
-
Guarding (muscle tension).
6. Diagnosis
- Clinical suspicion based on symptoms, physical examination and investigations.
-
Blood tests: Amylase (key diagnostic test), lipase, inflammatory markers (e.g CRP).
-
Imaging: Abdominal ultrasound, CT scan.
-
Abdominal X-ray: To exclude other causes.

-
Acute cholecystitis.
-
Peptic ulcer disease (including a perforated PU, and any abdominal viscus)
-
Gastroenteritis.
-
Inflammatory bowel disease.
7. Treatment
- There is no specific treatment.
-
Supportive care: Fluid resuscitation, analgesia, and nutritional support.
-
Endoscopic retrograde cholangiopancreatography (ERCP): For gallstone-related pancreatitis.
-
Surgery: For necrotising pancreatitis or complications.
When to seek medical attention with suspected acute pancreatitis
- Almost all patients should go to A&E
-
Severe abdominal pain.
-
Fever above 38.5°C.
-
Difficulty breathing.
8. Complications
-
Pancreatic necrosis: Death of pancreatic tissue.
-
Infection: Bacterial or fungal.
-
Pseudocyst: Fluid collection.
-
Abscess: Infected fluid collection.
-
Systemic inflammatory response syndrome (SIRS): Organ dysfunction.
9. Prognosis
10. Prevention
- Avoid excessive alcohol consumption.
- Manage underlying conditions: Gallstones (remove if more than one bad attack of acute cholecystitis), hypertriglyceridaemia.
- Vaccination: Against influenza and pneumococcus.