10 AKI (acute kidney injury) facts
AKI used to be called ‘Acute Renal Failure (or ARF)’. AKI is a simpler phrase in some ways; but there is no real injury, in a trauma sense.
We will now go through 10 in depth facts about AKI.
5 Key Points
- Acute Kidney Injury (AKI): a rapid loss of kidney function, resulting in the accumulation of waste products, electrolyte disturbances, and fluid imbalance
- AKI is common: Affects up to 20% of hospitalised patients
-
AKI is a marker of severity: Often reflects underlying critical illness
-
Mortality rates are high: Up to 50% of patients with severe (dialysis-requiring) AKI may die
-
Prevention is key: As 90% cases are prerenal (due to sepsis and dehydration), early treatment with IV fluids and antibiotics is important.
1. Definition
- Acute Kidney Injury (AKI) is a rapid loss of kidney function, resulting in the accumulation of waste products, electrolyte disturbances, and fluid imbalance
- AKI usually occurs over hours or days, and will usually require admission to hospital
- AKI affects both kidneys, and is different from Chronic Kidney Disease (CKD) which has different causes, and occurs over months or years.
Note 1. Primary problem: is not usually the kidneys themselves. They are usually reacting to an underlying current serious condition, such as dehydration, infection (sepsis) and nephrotoxic medication, after an operation. Therefore the patient’s medical condition will be dominated by the underlying disease (cause).
Note 2. Duration: for most people, AKI (if it causes ATN, see below) lasts about 10-14 days but can be 2 days or 3 months. If the patient is still in AKI at 3 months, we normally assume CKD has started.
Types
-
Prerenal AKI: Caused by decreased blood flow to the kidneys – e.g. dehydration, hypotension, vasodilatation
-
Intrinsic AKI: Caused by direct kidney damage – e.g. medication, interstitial nephritis, glomerulonephritis (rare)
-
Postrenal AKI: Caused by obstruction of urine flow – e.g. bladder outlet obstruction.
Why is AKI important?
- It is very common
- AKI will double the patient’s average length of stay, and increase the readmission rate; and dialysis-requiring AKI has a very high mortality
- 90% of cases are prerenal (see later) and due to dehydration and sepsis; so relatively easy to treat (and prevent)
- Around 65% of AKI starts in the community, before the patient comes to hospital. But 35% are acquired in hospital, especially after surgery and some x-rays (angiograms, CTs etc)
- 30% are due to prescribed drugs
- 15 million people in the UK have diabetes, which puts them at greater risk of AKI
- The annual cost of AKI-related inpatient care in England is estimated at £1 billion, around 1% of the NHS budget.
2. Epidemiology
-
AKI affects up to 20% of hospitalised patients
-
Incidence increases with age, diabetes, other comorbidities (e.g. CHF), and severity of illness
-
AKI is more common in ICU patients, with an incidence of up to 50%.
3. Risk factors
-
Age: Older adults are at higher risk
-
Comorbidities: Diabetes, hypertension, chronic heart failure (CHF), and liver disease
-
Medication: NSAIDs, ACE inhibitors, ARBs, and certain antibiotics (penicillins, cephalosporins, aminoglycosides)
-
Surgery: Major surgery, especially cardiac and vascular procedures
-
Sepsis: Infection and sepsis can cause AKI.
4. Causes
The causes of acute kidney injury can be divided into prerenal, renal and post-renal types. These phrases mean problems with the blood supply to the kidneys (pre), the kidneys themselves (renal), and the urine drainage pipes or bladder (post).
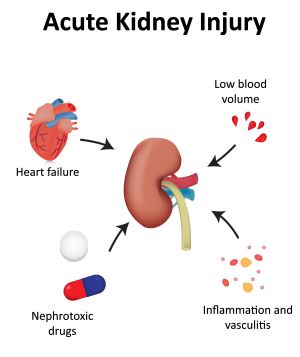
Pre-renal (90% of cases)
- Dehydration and infection (sepsis) is the commonest cause. Other causes include:
- Bleeding (haemorrhage)
- Cardiac failure
- Low blood pressure
- Liver failure
- Blockages to the (renal) arteries to the kidneys (renal artery stenosis).
Renal
- Tubulo-interstitial disease (TID)
- Acute Tubular Necrosis (ATN). This is the commonest TI cause. It is usually secondary to prolonged hypoperfusion (largely all the prerenal causes). In ATN, the kidney is pre-programmed (for reasons we don’t understand) to ‘close down’ (blood goes to it and from it, but it is not filtered) for 10-14 days, and then it ‘opens up’ and starts doing its normal job again. Dialysis may be required during this period
- Drugs toxic to the kidneys – e.g. NSAIDs, ACEi/ARBs, antibiotics (such as aminoglycosides like gentamicin), or chemotherapy (such as cisplatin) and the dye that is injected for CTs and other x-rays (contrast nephropathy)
- Autoimmune diseases (all rare), such as:
- Glomerulonephritis (GN) (inflammation of tiny filtering units in the cortex (outer area) of the kidney)
- Vasculitis (inflammation of small to medium sized blood vessels)
- Acute tubulointerstitial nephritis (TIN) (inflammation of tubes between the filtering units; in the medulla (inner area) of the kidney)
- Other: rhabdomyolysis, multiple myeloma, or haemolytic-uraemic syndrome (HUS; very rare)
Post-renal
- In men, it is usually due to enlargement of the prostate gland (benign (BPH) or malignant)
- In women, pelvic cancer is commonest cause
- Bladder cancer is another cause and can affect men and women.
Note. Renal stones are not a common cause of AKI, but can do – usually if you have one kidney.
5. Symptoms and signs
The symptoms are dominated by underlying cause. But here are some that can occur in any case.
- Oliguria (passing less urine), strangely, is not that common. Indeed the rate of urine production can even be increased
- Concentrated urine, or urine looking yellow/brown/red in colour; again, not that common
- Loss of appetite, feeling sick (nausea) or vomiting
- Feeling tired and short of breath
- Feeling confused, anxious and restless, or sleepy
- Swelling of your legs, around eyes, and other body parts.
Note. There may be no symptoms and it is picked up on a routine blood test.
Medical assessment
This involves the doctor asking you questions – especially related to your current condition (and surgery if you have had it), and what tablets you are on. This is followed by a careful examination, focusing on the amount of fluid in your body and your tummy. The blood pressure is very important.
Urine output
AKI is not usually determined by how much urine you make, as you can have quite severe AKI with normal (or even increased) urine output.
Complete anuria (no urine output) is rare but always very serious. It has only three causes: ‘vascular catastrophe’ (complete disruption of kidney arteries; pre-renal), acute severe glomerulonephritis (renal) or complete urine blockage (post-renal).
6. Diagnosis
-
Serum creatinine: Elevated levels indicate AKI
- Electrolytes: Abnormalities in potassium, sodium, and calcium levels
-
Urinalysis: Haematuria, proteinuria, and casts may be present.
Investigation
- A urine dipstick helps to identify a potential underlying cause. Blood and protein suggest an autoimmune ‘renal cause’
- Blood tests should include:
- U&Es; including creatinine, which is the best marker of kidney function; the higher the number the worse the function – 60-120 mcmol/L is normal
- Glucose, LFTs, and bone biochemistry (calcium, phosphate and parathyroid hormone (PTH))
- FBC, CRP, and blood cultures
- Renal immunology (in some patients)
- A special blood test called an ‘arterial blood gas (ABG)’ (taken from an artery at the wrist) if useful as it gives the doctor an idea of how unwell you are, and they will get the results back immediately
- Urinary ACR. If there is alot of urinary protein, a glomerular cause is likely
- A chest x-ray (looking for pulmonary haemorrhage (as part of a ‘pulmonary-renal syndrome’), as well as pulmonary oedema and pneumonia)
- An ultrasound scan of the kidneys, ureters and bladder is required in more severe cases; especially if there is no response to initial treatment, to check you have two kidneys and look for post-renal (obstructive) causes
- Rarely a kidney biopsy (removal of a piece of kidney) is required.
Differential diagnosis
-
Chronic kidney disease: Gradual decline in kidney function
-
Urinary tract obstruction: Blockage of urine flow.
7. Treatment
- Pre-renal – intravenous fluids and antibiotics
- Renal – stop drugs, and treatment of rare causes with strong drugs to suppress the immune system
- Post-renal – unblock the bladder with a urinary catheter; or other procedures and operations.
If this does not work, temporary dialysis may be required. The renal (kidney) team should be called to carry out this treatment, with transfer to their ward. A small number of more unwell patients will need intensive care.
Drug rationalisation
This is a very important part of treatment. Medications can both affect and be affected by the kidneys, so it’s important that medications are reviewed in cases of AKI.
Drugs to be potentially stopped (or dose reduced)
- ACEi and ARBs
- SGLT2 inhibitors
- Diuretics (if patient is dehydrated)
- NSAIDs
- Aminoglycoside antibiotics
- Potassium-sparing diuretics (due to risk of a high blood potassium (hyperkalaemia))
- Metformin (risk of lactic acidosis)
- Low-molecular weight heparin
- Opioids – e.g. morphine or codeine.
Note. Some of these drugs (especially the first three) will need to be restarted by the patient’s GP when they are better
8. Complications
-
Fluid overload: Pulmonary oedema, hypertension, and cardiac failure
-
Electrolyte disturbances: Hyperkalemia, hypokalaemia, and metabolic acidosis
-
Uraemic symptoms: Nausea, vomiting, and altered mental status
-
Infections: Increased risk of infections, especially pneumonia and sepsis
-
Malnutrition: Impaired nutritional status due to decreased appetite and altered metabolism
-
Cardiovascular events: Increased risk of myocardial infarction, stroke, and cardiac arrhythmias
-
Progression to chronic kidney disease (CKD): AKI can lead to CKD, especially in patients with pre-existing kidney disease
-
Increased mortality: AKI is associated with increased mortality rates, especially in critically ill patients.
9. Prognosis
The outlook is largely dependent on the outlook of the underlying condition, and stage of AKI (see below)
- Mortality. The mortality is high. Overall it is over 10% (double the ‘normal’ mortality for a medical admission); 30% if transferred to a renal ward, and 50% if dialysis is required there. If the patient is on ICU (and on ventilator) the mortality is higher again (70%)
- Length of hospital stay: AKI doubles length of hospital stay and increases readmission rate
- Renal recovery. Most patients recover (if they survive), and the kidney function usually returns to the baseline level. This usually happens in 10-14 days, and for most people by three weeks. A small number take upto 3 months. If the patient is on dialysis at 3 months, this is not a good sign, and you should start making plans for long-term dialysis or a kidney transplant.
- Repeat AKI episodes. Some patients (especially those with CKD3A or worse at baseline) are at risk of repeat AKI episodes which can lead worsening CKD.
Stages of AKI
Prognosis is largely determined by the prognosis of the underlying disease, and stage of AKI (higher stages have a worse prognosis)
- AKI Stage 1: Serum creatinine 1.5–1.9 times baseline
- AKI Stage 2: Serum creatinine 2.0–2.9 times baseline
- AKI Stage 3: Serum creatinine ≥ 3.0 times baseline.
Stage 1 is the mildest (best) form, and Stage 3 the most severe (worst) form.
Distinguishing AKI and CKD
Most patients with AKI look unwell, may have hyperkalaemia (potassium > 6.0 mmol/L), and are either already admitted for something else or need admission and rapid review.
Patients with Chronic (i.e. long term) Kidney Disease (CKD) usually look well, and may have other complications of CKD (e.g. anaemia, low calcium, high PTH etc).
Patients can have both, i.e. AKI on the background of CKD (‘AKI-on-CKD’).
10. Prevention
Inpatients
-
Optimise fluid status: Ensure adequate fluid intake and avoid dehydration (or fluid overload)
-
Monitor renal function: Regularly check serum creatinine and urine output
-
Avoid contrast-induced nephropathy: Use alternative imaging modalities or pretreat with N-acetylcysteine and hydration
-
Maintain adequate blood pressure: Avoid hypotension, especially in patients with pre-existing kidney disease
-
Provide nutritional support: Ensure adequate nutrition to prevent malnutrition and support renal function
-
Implement AKI prevention bundles: Use standardised care bundles to prevent AKI in high-risk patients.
Outpatients
- Sick Day Cards
- The primary aim is prevention of AKI through education of patients (making them aware of their higher AKI risk), regular medicines management reviews and ‘sick day guidance’
- Sick Day Cards should be given to vulnerable patients (especially the elderly on many drugs, with CKD).
- These ask the patient to stop a range of drugs – including Metformin, ACE/ARB, SGLT2is, NSAIDs and diuretics – for a few days if they are feeling unwell (especially septic, e.g. fever, gastroenteritis, UTI). They also need to be encouraged to drink more when they are unwell (especially if septic)
- These drugs usually need to be restarted 48 or more hours later, when better, and eating and drinking normally. Discuss that with the patient’s GP.
- Manage underlying conditions: Control blood pressure, blood sugar, and cholesterol levels.
Summary
We have described 10 AKI (acute kidney injury) facts. Most people will make a full recovery.
Other resources
There is more information on Acute Kidney Injury (AKI) (Acute Renal Failure) written by the renal team at UHCW, Coventry.
This is good doctors review article.
This is another simpler doctor’s article.
And this is a good video especially related to the classification and investigation of AKI: https://www.simpleosce.com/interpretation/disease-specific/acute-kidney-injury.php.
This article was reviewed by Rachael Lee, AKI Advanced Nurse Practitioner, UHCW Coventry.

