10 appendicitis facts
Key Points
-
Appendicitis is a surgical (and medical) emergency that requires prompt treatment.
-
It’s essential to have a high index of suspicion for appendicitis in patients presenting with abdominal pain.
- This is because atypical presentations are common.
-
A thorough history, physical examination, and imaging studies are crucial for accurate diagnosis.
-
Delayed treatment can lead to complications, such as perforation and peritonitis.
1. Definition
- Appendicitis is inflammation of the appendix, a small, finger-like pouch attached to the large intestine.
- The appendix has no known function, but it can become inflamed, leading to severe abdominal pain and potentially life-threatening complications.
The appendix is a small organ located in the lower right side of the abdomen. It is like a finger coming out of the side of the caecum; which is part of the right lower colon.

This means the appendix is usually (see below) in the right lower quadrant of the abdomen.
-
Acute appendicitis: Sudden onset of inflammation, usually requiring emergency surgery.
-
Chronic appendicitis: Recurrent or ongoing inflammation, often requiring medical management.
2. Epidemiology
- Appendicitis is a common condition, affecting approximately 1 in 1,000 people in the UK each year.
- It’s more common in young adults, with a peak incidence between 10-30 years old.
3. Risk Factors
-
Age: Young adults are more susceptible.
-
Sex: Males are more likely to develop appendicitis than females.
-
Family history: Having a family history of appendicitis increases the risk.
-
Obesity: Being overweight or obese increases the risk.
4. Causes
-
Obstruction of the appendix: Blockage of the appendix by stool, inflammation, or other debris.
-
Bacterial overgrowth: Increased bacterial growth in the appendix can lead to inflammation.
-
Abnormalities of the appendix: Anatomical abnormalities, such as a narrow appendix, can increase the risk.
5. Symptoms
-
Severe abdominal pain: Initially, the pain may be diffuse, colicky and central (around umbilicus), but it often localises to the right lower quadrant, and becomes constant in nature.
-
Nausea and vomiting.
-
Loss of appetite.
-
Fever’
-
Abdominal tenderness and guarding.
But importantly, the symptoms of appendicitis can vary. And it can be hard to detect appendicitis in young children, older people, people on steroids, and women of childbearing age.
As said above, even though it usually starts in the middle of the tummy, and is colicky (means comes and goes) in nature.
It then usually moves to the lower right side of the abdomen, and becomes constant. This most often occurs 12 to 24 hours after the illness starts.
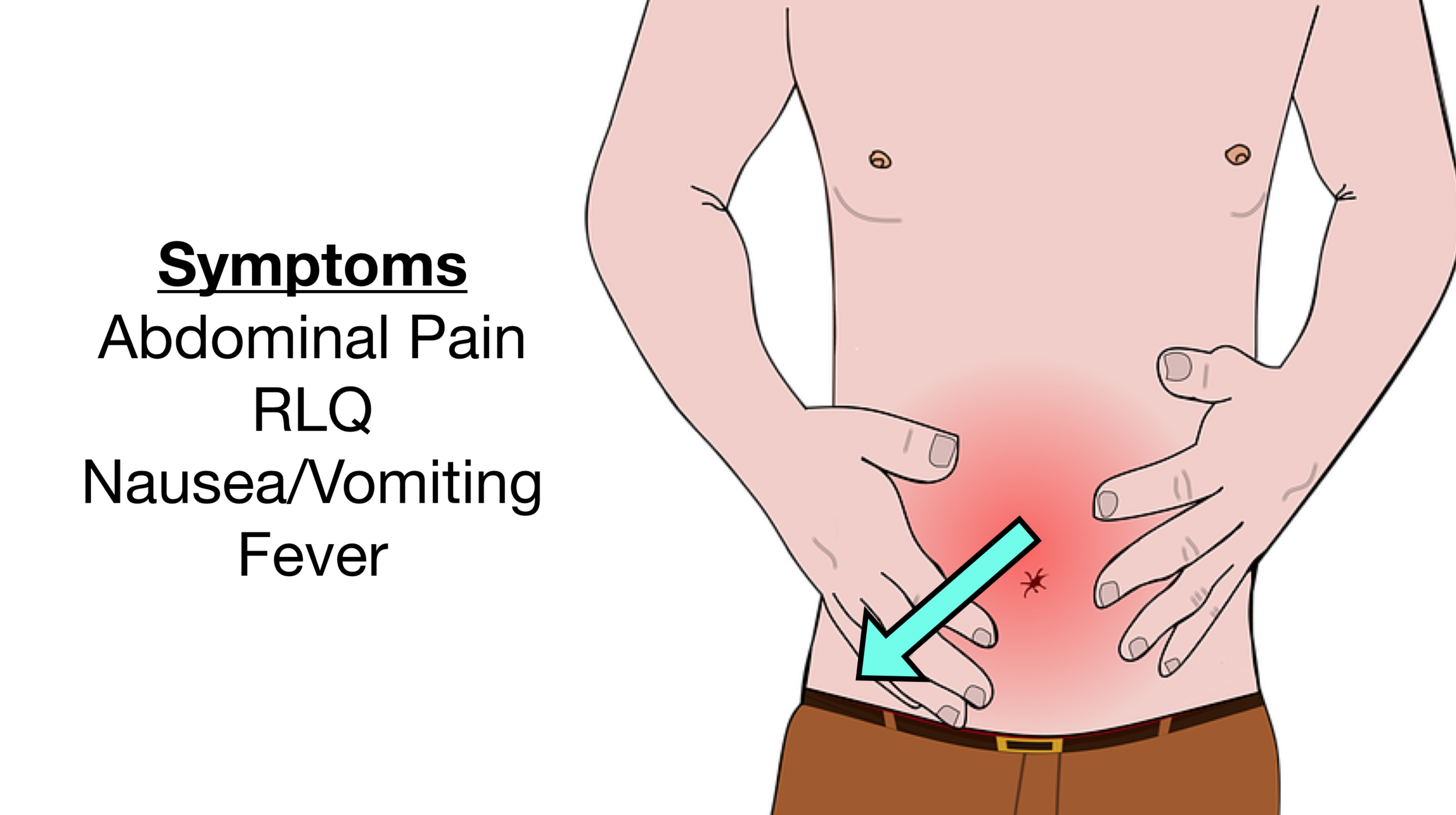
The pain and tenderness often finally settles on a spot directly above the appendix called McBurney point.
But. As they can point in many directions (or be on the left side in some people), this can give different clinical presentations – e.g. abdominal pain in different places.
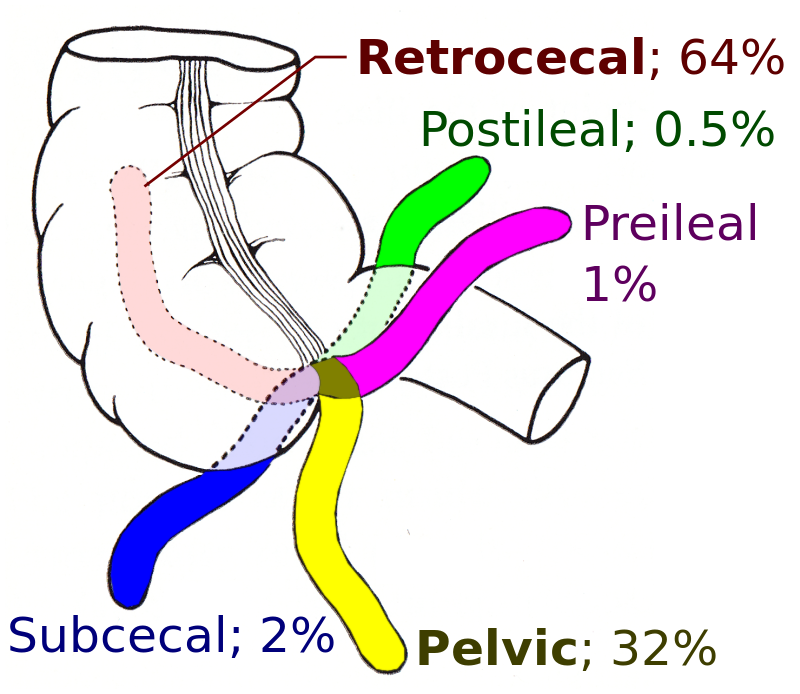 Different directions of the appendix
Different directions of the appendix
6. Diagnosis
-
Abdominal examination: To assess tenderness, guarding, and rebound tenderness.
-
Rectal examination: To check for tenderness and masses.
-
Laboratory tests: To evaluate for signs of infection, such as elevated white blood cell count, and CRP.
- Computed Tomography (CT) scan: To provide detailed images of the appendix and surrounding tissues. This is the best test.
-
Magnetic Resonance Imaging (MRI): To evaluate for complications, such as abscesses.
- Ultrasound: To visualise the appendix and surrounding structures.
-
Gastroenteritis.
-
Urinary tract infection (UTI).
-
Ovarian torsion.
-
Ectopic pregnancy.
-
Inflammatory bowel disease.
- Diverticular disease.
7. Treatment
-
Surgical removal of the appendix (appendicectomy): Either open or laparoscopic surgery.
-
Antibiotics: To treat bacterial infections and prevent complications.
-
Pain management: To control pain and discomfort.
-
Severe abdominal pain.
-
Vomiting.
-
Fever.
-
Abdominal tenderness and guarding.
8. Complications
-
Perforation: Rupture of the appendix, leading to peritonitis.
-
Peritonitis: Inflammation of the lining of the abdominal cavity.
-
Abscesses: Collections of pus that can form in the abdomen.
-
Sepsis: Life-threatening condition caused by bacterial infection.
9. Prognosis
- The prognosis for appendicitis is generally good if treated promptly. However, delayed treatment can lead to complications and increased morbidity.
10. Prevention
- Whilst there is no known way to prevent appendicitis, maintaining a healthy lifestyle may (may) reduce the risk, e.g.
- Eating a balanced diet, with high-fibre foods may help prevent constipation. Whether this reduces the risk of appendicitis is not known.
Summary
We have described 10 facts about appendicitis. We hope it has been helpful.
Other resource
MyHSN has more on the symptoms of appendicitis and Patient information: 10 appendicitis facts

