10 BPH (benign prostatic hyperplasia) facts
In this article we will describe 10 facts about BPH (benign prostatic hyperplasia).
Key Points
- Benign prostatic hyperplasia (BPH), also known as prostate enlargement, is a noncancerous condition that causes the prostate gland to enlarge
- It is more than common. It is normal. 20-30% of men aged 50-59, 50-60% of men aged 60-69, and 80-90% of men aged 80-89 years
- Characterised by enlarged prostate gland, leading to lower urinary tract symptoms (LUTS)
-
Diagnosis based on symptoms, digital rectal examination (DRE), and investigations like ultrasound and uroflowmetry
-
Treatment options include lifestyle modifications, medications, and surgery.
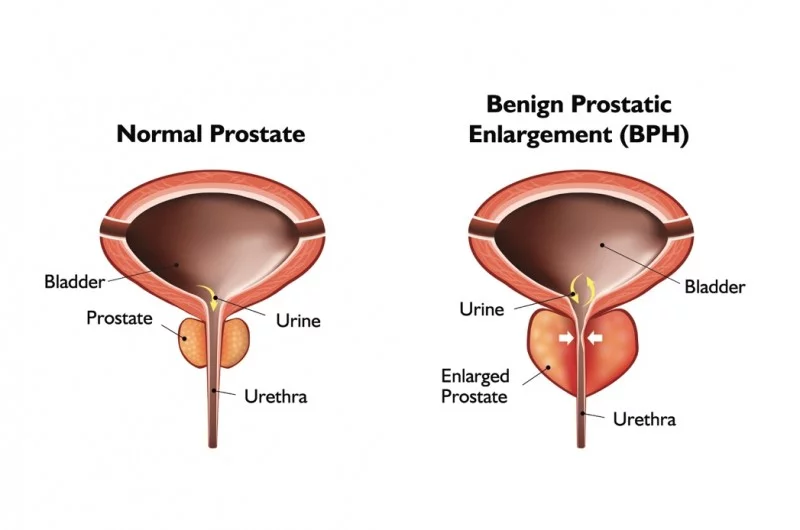
1. Definition
- Benign prostatic hyperplasia (BPH), also known as benign prostatic enlargement, is a noncancerous condition that causes the prostate gland to enlarge
- As the prostate gland surrounds the urethra, it affects urine flow.
- It is a common condition affecting men, particularly in the fifth decade of life and beyond.
Types
BPH can be classified into several types based on the severity of symptoms and prostate size:
-
Small gland BPH: Prostate volume <30g, minimal symptoms
-
Large gland BPH: Prostate volume ≥30g, moderate to severe symptoms
-
Simple BPH: Symptomatic BPH without complications
-
Complicated BPH: BPH with associated complications (e.g. urinary retention, recurrent urinary tract infections, UTIs).
2. Epidemiology
- It is more than common. It is normal
-
Prevalence increases with age: 20-30% of men aged 50-59, 50-60% of men aged 60-69, and 80-90% of men aged 80-89
-
Estimated 12 million men affected in the UK
-
Projected increase in prevalence due to aging population.
3. Risk Factors
-
Age: risk increases after 50 years
-
Family history: first-degree relatives with BPH
-
Ethnicity: higher prevalence in African and Afro-Caribbean men
-
Obesity, metabolic syndrome, and diabetes
-
Hormonal imbalance (testosterone, dihydrotestosterone).
4. Causes
-
Hormonal changes: increased dihydrotestosterone (DHT) levels stimulate prostate growth
-
Cellular changes: proliferation of stromal and epithelial cells
-
Inflammation and oxidative stress.
5. Symptoms
-
Lower urinary tract symptoms (LUTS)
-
Urinary frequency and urgency
- Weak urine flow
-
Straining to urinate, dribbling post urination
-
Feeling of incomplete bladder emptying
- Nocturia
-
-
Additional symptoms: Painful urination (dysuria), blood in urine or semen
6. Diagnosis
-
Medical history and physical examination (DRE)
-
Symptom scoring systems (e.g. International Prostate Symptom Score, IPSS).
Investigation
- Urine dipstick
- Blood tests:
- U+E (renal function)
- Prostate-specific antigen (PSA; for prostate cancer); false positive and negative tests occur
- Uroflowmetry: measures urine flow rate and pattern; and post-void residual urine volume
- Ultrasound (transrectal or transabdominal): assesses prostate size, shape, and bladder wall thickness
- Cystoscopy: also examines urethra and bladder.
Differential Diagnosis
-
Prostate cancer
-
Prostatitis (inflammatory or infectious)
-
Bladder cancer
-
Overactive bladder
-
Neurogenic bladder.
7. Treatment
-
Lifestyle modifications
-
Fluid management
-
Bladder training
-
Pelvic floor exercises
-
Avoidance of irritants (caffeine, alcohol).
-
-
Medications
-
Alpha-blockers (e.g. tamsulosin)
-
5-alpha-reductase inhibitors (e.g. finasteride)
-
Phosphodiesterase inhibitors (e.g. tadalafil).
-
-
Surgery
-
Transurethral resection of the prostate (TURP)
-
Open prostatectomy
-
Laser therapy.
-

Transurethral resection of the prostate (TURP)
When to see a doctor with suspected BPH
-
Symptoms persist or worsen
-
Difficulty starting or stopping urination
-
Painful urination
-
Blood in urine (haematuria) or semen
-
Recurrent urinary tract infections (UTIs).
8. Complications
- Urinary incontinence
-
Urinary retention
- AKI, CKD or AKI on CKD due to obstructive nephropathy (usually with bilateral hydronephrosis)
- Recurrent urinary tract infections
- Bladder stones
-
Erectile dysfunction (ED).
9. Prognosis
-
BPH is a chronic condition, but symptoms can be effectively managed
-
Early treatment prevents complications
-
Regular monitoring essential for disease progression.
10. Prevention
- No known way of reliably preventing
- It may help to: maintain a healthy weight, exercise regularly, have a balanced diet (fruit, vegetables, whole grains), and limit caffeine and alcohol intake.
Summary
We have described 10 facts about BPH (benign prostatic hyperplasia). We hope it has been helpful.

