10 common kidney diseases (with photos)
In this article we will describe 10 common kidney diseases, and include relevant photos.
1. Chronic Kidney Disease (CKD)
A progressive loss of kidney function over months or years (or abnormal structure), often associated with diabetes and hypertension. Management focuses on slowing progression and addressing complications.
- Definition: CKD is a gradual loss of kidney function over time, leading to the buildup of waste products and excess fluid in the body
- Causes: Include diabetes (20%), renovascular disease (TVD), glomerulonephritis (GN), tubulointerstitial disease (TID), polycystic kidney disease (PKD) and obstructive nephropathy (ON). In 30%, the cause is unknown with small kidneys.
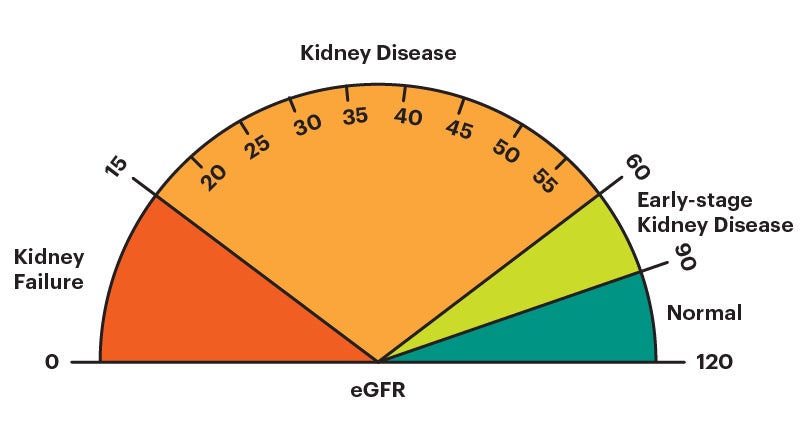
- Stages: CKD is divided into five stages based on glomerular filtration rate (GFR)
- Stage 1: Kidney structural damage with a normal or increased glomerular filtration rate (GFR) of 90 ml/min or higher (i.e normal function)
- Stage 2: Mild reduction in GFR of 60-89 ml/min
- Stage 3a: Moderate reduction in GFR of 45-59
- Stage 3b: Moderate to severe reduction in GFR of 30-44
- Stage 4: Severe reduction in GFR of 15-29
- Stage 5: Kidney failure with a GFR of less than 15 or dialysis.
- Symptoms: Early stages may be asymptomatic, but advanced stages can cause fatigue, leg swelling and shortness-of-breath (SOB), itching, nausea, vomiting, restless legs, difficulty concentrating and sleeping.
- Treatment: Lifestyle modification (diet, weight loss, exercise), medication (blood pressure and anti-proteinuric medication, diabetes management if needed); and in severe cases, dialysis or kidney transplantation.
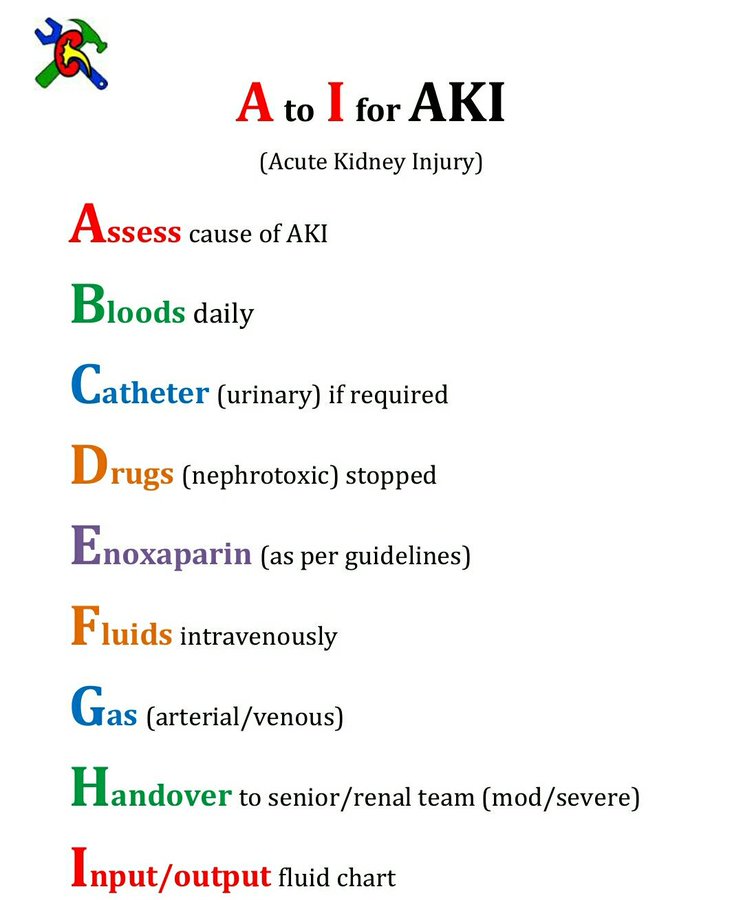
2. Acute Kidney Injury (AKI)
A rapid decline in renal function, commonly due to dehydration/sepsis, medication, post-op or obstructive causes. Prompt identification and treatment of the underlying cause is crucial to improve outcomes.
- Definition: Rapid loss of kidney function, occurring within hours or days, leading to the accumulation of waste products/excess fluid and electrolyte imbalances. May be oliguric, normo-uric or polyuric.
- Types and causes
- Types: Pre-renal, renal and post-renal
- Causes: Dehydration/sepsis, medication (e.g. NSAIDs, ACE/ARBs, antibiotics), and post-op or post-procedure (e.g. angiogram).
- Stages: AKI is classified into three stages based on serum creatinine levels and urine output:
- Stage 1: Mild increase in serum creatinine
- Stage 2: Moderate increase in serum creatinine
- Stage 3: Severe increase in serum creatinine or acute kidney failure.
- Symptoms: May include decreased urine output (oliguria) or fluid overload, electrolyte disturbance, and those of underlying cause.
- Treatment: Involves identifying and addressing underlying cause(s), fluid management, medication adjustment (often stopping nephrotoxic medication); and in severe cases, dialysis (or supportive care), which may be in an intensive care unit (ICU).
3. Polycystic Kidney Disease (PKD)
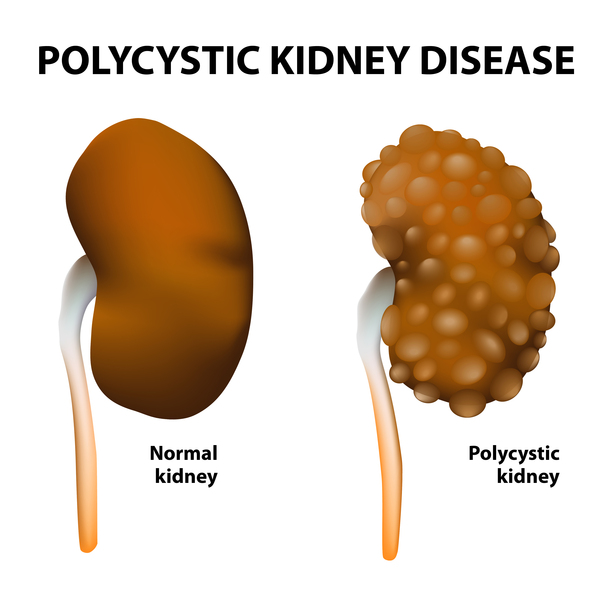
An inherited disorder characterised by the growth of numerous cysts in the kidneys, leading to enlarged kidneys and impaired function. Supportive care and monitoring are key, as there’s no cure.
- Definition: Genetic disorder characterised by the growth of numerous fluid-filled cysts in the kidneys; leading to kidney enlargement and potentially kidney failure. Cysts also occur in the liver and many other organs. Non-cystic features in the brain, heart and other organs also occur.
- Types: Two main types:
- Autosomal Dominant PKD (ADPKD): Most common form, usually diagnosed in adulthood.
- Autosomal Recessive PKD (ARPKD): Rare form, typically diagnosed in infancy or childhood.
- Symptoms
- Loin, abdominal or back pain
- Haematuria (blood in urine; microscopic or macroscopic)
- Hypertension (high blood pressure)
- Of complications (e.g. subarachnoid haemorrhage, SAH).
- Treatment
- Blood pressure control
- Pain management
- Antibiotics for infections
- Surgical intervention (cyst drainage or kidney transplantation)
- Lifestyle modification (diet, exercise, weight loss).
- Complications
- CKD/ESRF
- Cyst rupture, bleeding or infection
- UTIs
- Kidney stones
- Liver cysts
- Of non-cystic features – e.g. SAH (berry aneurysm).
4. Kidney Stones

These are solid concretions of dissolved minerals in urine, often causing severe pain (and sometimes urinary obstruction). Treatment may include pain management, lithotripsy, or surgical removal.
- Definition: Kidney stones are small, hard mineral deposits that form inside the kidneys when there is an imbalance of water, salts and other substances in the urine.
- Types: Common types of kidney stones include:
- Calcium oxalate stones
- Uric acid stones
- Cystine stones
- Struvite stones (related to urinary tract infections, UTIs).
- Risk factors
- Dehydration
- Certain foods (e.g. high-oxalate foods)
- Family history
- Medical conditions (e.g. gout, chronic kidney disease (CKD))
- Obesity.
- Symptoms
- (Often severe) loin, abdominal or back pain (renal colic)
- Nausea and vomiting
- Frequent or painful urination
- Haematuria (blood in urine; microscopic or macroscopic)
- Fever (indicating infection).
- Treatment: Depending on stone size and location, treatment may include:
-
Drinking plenty of water to pass small stones
-
Pain relief medication
-
Medical procedures (extracorporeal shock wave lithotripsy, ureteroscopy)
-
Surgery (percutaneous nephrolithotomy or open surgery).
-
5. Glomerulonephritis

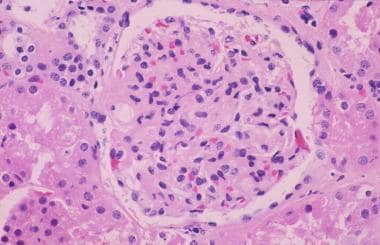
This is a glomerulus in a patient with rapidly progressive glomerulonephritis (RPGN), with a crescentic pathology. Note the crescent of abnormal cells on the right side of the glomerulus
Glomerulonephritis (GN) is an autoimmune inflammation of the glomeruli, that can present in many ways from asymptomatic with microhaematuria or hypertension to proteinuria/nephrotic syndrome, or AKI/CKD. Treatment varies depending on the aetiology but may include immunosuppressive therapy.
-
Definition: Glomerulonephritis is inflammation of the glomeruli, the tiny filters within the cortex (outer layer) of the kidneys responsible for removing waste and excess fluids. There are a million in each kidney. It affects both kidneys.
-
Types: Main categories include:
-
Proteinuric GNs: Minimal Change Disease (MCD), Focal Segmental Glomerulosclerosis (FSGS) and Membranous Nephropathy (MN))
-
Less proteinuric GNs: IgA nephropathy, Post-infectious GN, Mesangiocapillary GN, Rapidly progressive GN (most aggressive form).
-
-
Causes
- Renal-limited autoimmune disease (see above)
-
Systemic autoimmune disease (e.g. lupus, vasculitis)
-
Infections (e.g. post-streptococcal GN; Hep B/C/HIV)
-
Toxins and medications (e.g. gold/penicillamine)
-
Genetic disorders (e.g. Familial IgA nephropathy).
-
Symptoms
-
Haematuria (blood in urine; microscopic or macroscopic)
-
Proteinuria/nephrotic syndrome (excess protein in urine)
Note: significant proteinuria suggests a glomerular disease -
Oedema (swelling)
- Of AKI/CKD
-
Hypertension.
-
-
Treatment: Depending on the underlying cause and severity, treatment may involve:
- Corticosteroids and immunosuppressants
-
Antibiotics or antifungals for infection (e.g. of removing cause)
-
Blood pressure control
- Anti-proteinuric medication: ACE/ARB and SGLT2i
- Dialysis or kidney transplantation in severe cases.
6. Urinary Tract Infections (UTIs)

UTIs can affect any part of the urinary tract: kidney (pyelonephritis), bladder (cystitis), urethra (urethritis) and prostate (prostatitis) in a man (prostatitis).
- Definition: UTI is an infection occurring in any part of the urinary system, including kidneys, ureters, bladder, urethra, or prostate (in a man). Patients may be asymptomatic or have a wide range of symptoms, according to which part involved.
- Causes
- Bacteria (e.g. E. coli, Klebsiella, Pseudomonas)
- Fungi (e.g. Candida)
- Parasites
- Sexually transmitted disease (STD)
- Catheterisation or medical procedures.
- Risk factors
- Female sex
- Sexual activity
- Pregnancy
- Diabetes
- Obesity.
- Symptoms
- Dysuria (painful urination)
- Frequent or urgent urination
- Cloudy or strong-smelling urine
- Haematuria (blood in urine; microscopic or macroscopic)
- Loin, abdominal, pelvic or back pain
- Treatment
- Antibiotics for bacterial infections
- Antifungal medication for fungal infections
- Chase urine culture (MSU) tests to determine best antibiotic.
7. Nephrotic syndrome
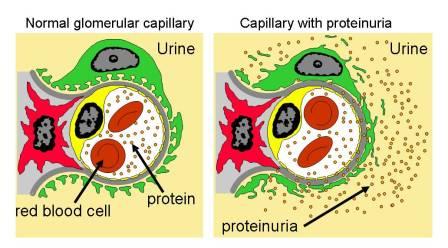
- Definition: Nephrotic syndrome is a chronic/subacute kidney disorder characterised by excessive loss of protein in the urine, leading to low albumin levels, oedema, venous thromboembolism and hyperlipidaemia.
- Causes
- Primary autoimmune renal disease – usually chronic glomerulonephritis; especially proteinuric forms, e.g. Minimal Change Disease (MCD), Focal Segmental Glomerulosclerosis (FSGS) and Membranous Nephropathy (MN)
- Secondary to systemic disease – e.g. Diabetic nephropathy, Amyloid and Lupus nephritis.
- Symptoms
- Severe oedema (swelling)
- Proteinuria (excess protein in urine)
- Hypoalbuminaemia (low albumin levels)
- Hyperlipidemia (high cholesterol)
- Weight gain.
- Treatment: Depending on the underlying cause, treatment may involve:
- Treat underlying cause (e.g. diabetic control)
- Corticosteroids and immunosuppressants
- Blood pressure control
- Anti-proteinuric medication: ACE/ARB and SGLT2i
- Diuretics
- Statins
- Anticoagulation.
- Complications
- Infection
- DVT/PE (and other venous thromboses)
- CKD/ESRF
- Cardiovascular disease
- Electrolyte imbalance.
8. Obstructive nephropathy (ON)/hydronephrosis
Dilation of the renal pelvis and calyces due to obstruction of urine flow. The primary approach involves relieving the obstruction, often through surgical means. Bilateral urinary obstruction, if untreated, can lead to AKI or CKD (called urinary retention)/ESRF.
-
Definitions: Obstructive nephropathy (ON) means renal dysfunction due to obstruction of the urinary tract (preventing urine from draining) – both kidneys are affected. Hydronephrosis is a condition where one (or both) kidneys swell due to the accumulation of urine, usually caused by an obstruction in the urinary tract.
-
Causes
-
Kidney stones
-
Tumours or cysts
- Prostatic enlargement (men)
-
Ureteropelvic junction (PUJ) obstruction
- Rare: retroperitoneal fibrosis (RPF).
-
-
Symptoms
- Often asymptomatic
-
Loin, abdominal or back pain
-
Nausea and vomiting
-
Fever
-
Haematuria (blood in urine; microscopic or macroscopic)
-
Frequent urination.
- Treatment: Depending on the underlying cause, treatment may involve:
-
Surgical removal of obstruction (e.g. kidney stones)
-
Endoscopic procedures (e.g. stenting)
-
Percutaneous nephrostomy (drainage tube)
-
Antibiotics for infection
-
Pain management.
-
- Complications
-
Kidney damage or scarring
-
Infection (pyelonephritis)
-
AKI or CKD/ESRF
-
Sepsis
-
Recurrent obstruction.
-
9. IgA Nephropathy (Berger’s disease)
IgA nephropathy – there are too many mesangial cells, indicating infection.
A form of chronic (sometimes acute) glomerulonephritis with IgA deposition in the glomeruli, often presenting with recurrent macrohaematuria. Management focuses on controlling blood pressure and proteinuria, and using immunosuppressive therapy if necessary.
-
Definition: IgA nephropathy, also known as Berger’s disease, is an autoimmune kidney disease characterised by the deposition of IgA antibodies in the glomeruli, leading to inflammation and kidney damage. It overlaps with Henoch–Schönlein purpura (HSP), when it is known as Henoch–Schönlein nephritis (HSN).
-
Causes and risk factors
-
Genetic predisposition
-
Infections (e.g. upper respiratory tract infections, URTIs)
-
Gastrointestinal diseases (e.g. gastroenteritis, coeliac disease)
-
High alcohol use
-
Family history (occasionally familial).
-
-
Symptoms
- Often asymptomatic
-
Haematuria (blood in urine; microscopic or macroscopic)
-
Of proteinuria/nephrotic syndrome (excess protein in urine)
-
Loin, abdominal or back pain
-
Hypertension.
-
Treatment
- Some patients require no treatment
- Blood pressure control
-
Anti-proteinuric medication: ACE/ARB and SGLT2i
- Corticosteroids and immunosuppressants (in some)
-
Fish oil supplements (omega-3 fatty acids)
-
Dialysis/kidney transplantation in advanced cases.
-
Complications
-
CKD/ESRF
-
Nephrotic syndrome
-
Hypertension
-
Increased risk of cardiovascular disease.
-
10. Diabetic Nephropathy

Diabetic nephropathy: characteristic Kimmelstiel-Wilson lesions are arrowed
Kidney damage caused by long-term poorly controlled diabetes, often presenting with proteinuria and progressive renal dysfunction. Managing blood pressure and proteinuria (and possibly tight glycaemic control) are essential in slowing progression.
-
Definition: Diabetic nephropathy, also known as diabetic kidney disease, is a microvascular complication of diabetes causing kidney damage and potentially leading to kidney failure.
-
Stages/types (Mogensen classification):
-
Stage 1: Hyperfiltration and glomerular hypertrophy
-
Stage 2: Microalbuminuria
-
Stage 3: Macroalbuminuria
-
Stage 4: CKD (decreased GFR)
-
Stage 5: End-stage renal failure (ESRF).
-
-
Risk factors
-
Duration of diabetes
-
Poor blood glucose control
-
Hypertension
-
Family history
-
Obesity.
-
-
Symptoms
-
Microalbuminuria (small amounts of albumin in urine) – asymptomatic
-
Of proteinuria/nephrotic syndrome (excess protein in urine)
-
Of CKD.
-
-
Treatment
-
Tight blood glucose control
-
Blood pressure control
- Anti-proteinuric medication: ACE/ARB and SGLT2i
-
Diuretics and fluid management
-
Dialysis/kidney transplantation in advanced cases.
-
Summary
We have described 10 common kidney diseases, and included relevant photos. We hope it has been helpful.