10 endometriosis facts

In this article we will describe 10 endometriosis facts.
Key Points
- Endometriosis is a chronic, often painful condition where tissue similar to the endometrium grows outside the uterus.
- Common symptoms include dysmenorrhoea, chronic pelvic pain, and infertility.
- Diagnosis is often delayed due to varied symptoms, with an average delay of 7-8 years.
- Treatment focuses on pain relief, hormonal therapies, and surgery in severe cases.
- Early diagnosis and management can improve quality of life and reduce the risk of complications such as infertility.
1. Definition
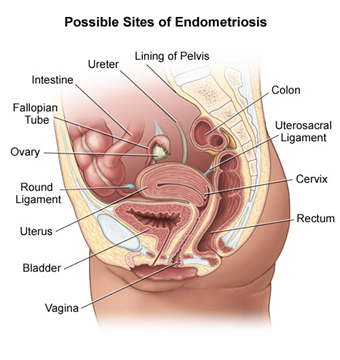
- Endometriosis is a gynecological disorder characterized by the presence of endometrial-like tissue outside the uterus, commonly on the ovaries, fallopian tubes, pelvic peritoneum, and other pelvic structures.
- This ectopic tissue responds to hormonal changes during the menstrual cycle, leading to inflammation, pain, and the formation of adhesions.
2. Epidemiology
- Prevalence: Endometriosis affects approximately 1 in 10 women of reproductive age, equating to around 1.5 million women in the UK. It is also found in 20-50% of women with infertility, and 70-90% of those with chronic pelvic pain.
- Age Distribution: Most commonly diagnosed in women aged 25-35 years but can occur in adolescents and persist into menopause.
- Delay in Diagnosis: On average, there is a delay of 7-8 years from symptom onset to diagnosis due to the non-specific nature of symptoms and lack of awareness.
3. Risk factors
- Family history of endometriosis (first-degree relatives)
- Early menarche (before age 11) or late menopause
- Short menstrual cycles (<27 days) or heavy, prolonged periods
- Nulliparity (never having given birth)
- Low body mass index (BMI)
- Anatomical abnormalities that obstruct menstrual flow
4. Causes
The exact cause of endometriosis remains unknown, but several theories exist:
- Retrograde Menstruation: The most widely accepted theory, where menstrual blood flows backward through the fallopian tubes into the pelvic cavity, depositing endometrial cells outside the uterus.
- Coelomic Metaplasia: Transformation of peritoneal cells into endometrial-like cells due to environmental or hormonal factors.
- Immune System Dysfunction: An impaired immune response may fail to clear ectopic endometrial tissue, allowing it to grow.
- Genetic Factors: A genetic predisposition may increase the risk of developing endometriosis, especially if close family members are affected.
5. Symptoms
- Dysmenorrhea: Painful menstrual cramps, often severe and worsening over time.
- Chronic Pelvic Pain: Non-menstrual pelvic pain that may radiate to the lower back and legs.
- Dyspareunia: Pain during or after sexual intercourse.
- Menstrual Irregularities: Heavy menstrual bleeding (menorrhagia) or spotting between periods.
- Infertility: Up to 30-50% of women with endometriosis may have difficulty conceiving.
- Other Symptoms: Painful bowel movements, urinary symptoms (dysuria, frequency), and bloating, particularly during menstruation.
Endometriosis most commonly involves the ovaries, fallopian tubes and the tissue lining of the pelvis. Rarely, endometrial-like tissue may be found outside the pelvis.
6. Diagnosis
Diagnostic criteria
- Clinical Diagnosis: Based on history and physical examination, particularly in patients with chronic pelvic pain, dysmenorrhea, or infertility.
- Definitive Diagnosis: Requires visual confirmation of endometriotic lesions, typically through laparoscopy, and histopathological biopsy.
Investigation
- Pelvic Examination: May reveal tenderness, nodularity, or pelvic masses (e.g., endometriomas).
- Transvaginal Ultrasound (TVUS): Useful in identifying ovarian endometriomas (chocolate cysts) but less effective in detecting smaller or superficial lesions.
- Magnetic Resonance Imaging (MRI): Provides detailed imaging, particularly for deep infiltrating endometriosis.
- Laparoscopy: The gold standard for diagnosis, allowing direct visualisation of lesions, and can also facilitate biopsy and treatment during the procedure.
- Serum CA-125: May be elevated in endometriosis but lacks specificity and sensitivity for diagnosis. Not routinely used but can assist in monitoring disease progression.
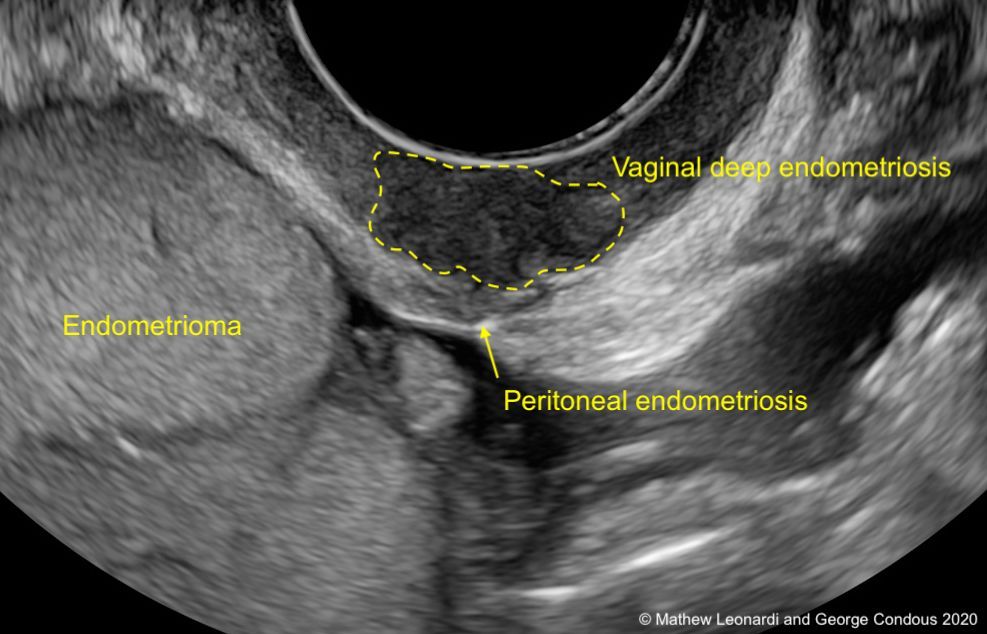 An ultrasound showing endometriosis
An ultrasound showing endometriosis
Differential diagnosis
- Pelvic Inflammatory Disease (PID): Can present with chronic pelvic pain and dyspareunia.
- Irritable Bowel Syndrome (IBS): Abdominal pain, bloating, and changes in bowel habits, which may overlap with gastrointestinal symptoms of endometriosis.
- Ovarian Cysts: Simple or complex cysts may cause pelvic pain.
- Uterine Fibroids: Menorrhagia and pelvic pain are common in fibroids, similar to endometriosis.
- Interstitial Cystitis: Chronic bladder pain and urinary symptoms.
7. Treatment
Pharmacological
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): First-line for pain relief, particularly for dysmenorrhea.
- Hormonal Therapy: Aims to suppress ovulation and reduce menstrual bleeding.
- Combined Oral Contraceptives (COCs): Effective in managing pain and regulating menstrual cycles.
- Progestins (e.g., Medroxyprogesterone, Norethisterone): Suppress endometrial growth.
- Gonadotropin-Releasing Hormone (GnRH) Agonists: Induce a hypoestrogenic state, reducing endometriotic lesions (use is limited due to side effects like bone loss).
- GnRH Antagonists: Newer agents that suppress ovarian function with fewer side effects than agonists.
- Levonorgestrel-Releasing Intrauterine System (LNG-IUS): Provides localized progestin release, reducing menstrual bleeding and pain.
Surgical
- Laparoscopic Excision or Ablation: Removal or destruction of endometriotic lesions can relieve pain and improve fertility. Preferred for patients who do not respond to medical treatment or have severe symptoms.
- Hysterectomy: Considered in severe cases where other treatments have failed, particularly for women who do not wish to conceive. Oophorectomy may also be performed if ovarian involvement is significant.
Supportive
- Lifestyle Modifications: Regular exercise, a balanced diet, and stress management can help manage symptoms.
- Pain Management: Referral to a pain specialist may be beneficial for patients with chronic pelvic pain.
- Psychological Support: Addressing mental health, including anxiety and depression, is crucial as chronic pain can significantly affect quality of life.
8. Complications
- Infertility: One of the most significant complications, affecting up to 50% of women with endometriosis. Adhesions and scarring can interfere with ovum release and fallopian tube function.
- Chronic Pain: Persistent pain even after treatment can impact physical, mental, and social well-being.
- Endometriomas: Cystic ovarian masses that can cause ovarian torsion or rupture.
- Adhesions: Scar tissue may form between pelvic organs, leading to chronic pain and bowel obstruction.
- Malignant Transformation: Rarely, endometriosis-associated ovarian cancers can develop, particularly in long-standing untreated cases.
9. Prognosis
- Symptom Variability: Prognosis varies widely depending on symptom severity, location, and response to treatment. While endometriosis is a chronic condition, many women can manage their symptoms effectively with a combination of medical and surgical approaches.
- Fertility Outcomes: Fertility may be improved with surgical management, particularly if adhesions or endometriomas are removed. Assisted reproductive technologies (ART), such as in vitro fertilization (IVF), may also be necessary for some women.
10. Prevention
- Primary Prevention: No established methods to prevent endometriosis; awareness and early symptom recognition are key to reducing the impact of the disease.
- Secondary Prevention: Early diagnosis and appropriate treatment can help control symptoms and prevent disease progression, thereby reducing the risk of complications such as infertility and chronic pain.
Patient information
Why can there be a delay in the diagnosis?
A lack of awareness of what endometriosis is, combined with a general belief that many of the symptoms are ‘normal’, often results in a long delay between when a woman first experiences symptoms, and when she is diagnosed and begins treatment.
Also endometriosis can be similar to:
- Other conditions that can cause pelvic pain, such as pelvic inflammatory disease (PID) or ovarian cysts
- Irritable bowel syndrome (IBS), a condition that causes bouts of diarrhoea, constipation and abdominal cramping. IBS can accompany endometriosis, which can complicate the diagnosis.
All of this can lead to diagnostic confusion.
Remember severe period pain isn’t normal
Period (menstruation) pain bad enough to interfere with your daily life (e.g. going to school or work, or taking part in day-to-day activities) is not normal. You should seek help from your doctor and ask about what’s causing your pain.
Endometriosis does not equal infertility
Many young women are given the impression that having endometriosis will mean they will be infertile (unable to conceive a baby). Whilst this may be the case, many women with endometriosis do go on to have children.
Pregnancy doesn’t cure endometriosis
Pregnancy, like hormonal drug treatments, may temporarily stop the symptoms of endometriosis, but doesn’t cure it – symptoms usually recur after the birth of the baby.
Summary
We have described 10 endometriosis facts. We hope you understand it better now.
Other resources
(For patients) Endometriosis UK has a:
Directory of local support groups
Helpline (0808 808 2227)
Webchat.
And an online community on HealthUnlocked for women affected by the condition.
MyHSN endometriosis podcast (2024) – 11 min, 35 sec
Top Tip
Endometriosis is found in 20-50% of women with infertility, and 70-90% of those with chronic pelvic pain. Diagnosis is often delayed. Think of it.