10 back pain facts
Back pain is normal.
Most humans have or have had it. In fact, 80% of the population have it at some point in their lifetime. And it is responsible for 40% of all lost work days.
Key Points
- High Prevalence: Approximately 80% of UK adults experience back pain at some point, contributing to significant NHS burden.
- Causes: Include mechanical, systemic, and psychological factors – requiring multidisciplinary care.
- Chronicity and Disability Risk: Chronic back pain is a leading cause of disability in the working-age population, responsible for 40% of lost work days.
- Preventive Focus: Lifestyle and ergonomic modifications can reduce recurrence and chronicity.
1.Definition
Back pain encompasses pain or discomfort localized between the neck and the sacral region, which can further be classified by duration:
- Acute Back Pain: Lasts less than six weeks.
- Subacute Back Pain: Persists from six to twelve weeks.
- Chronic Back Pain: Extends beyond twelve weeks.
These classifications inform diagnosis and treatment strategies, helping clinicians identify risk of progression to chronic pain.
2. Epidemiology
- In the UK, back pain affects around 8 million adults yearly, with chronic back pain being a leading cause of work-related disability and economic burden.
- It affects 80% of people at some point in their lives
- Back pain is more prevalent among older adults and women and disproportionately affects those in physically demanding occupations.
3. Risk Factors
Risk factors for back pain include:
- Age and Gender: Degenerative changes increase with age; women may be more susceptible due to osteoporosis and musculoskeletal structure.
- Occupation: Physically demanding jobs and demographic factors increase risk.
- Lifestyle: Smoking, obesity, and low physical activity are significant risk factors.
- Psychosocial Factors: Stress, depression, and low job satisfaction may contribute to chronicity and increased perception of pain.
4. Causes
Back pain can arise from several aetiological categories:
- Mechanical Back Pain: Common causes include herniated discs, facet joint disorders, and ligament injuries, and lumbar strain.
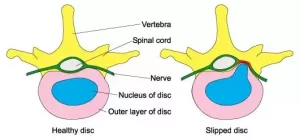 Prolapsed disc
Prolapsed disc

Spinal MRI: Prolapsed disc touching spinal nerves (not all patients need an MRI). A common cause of back pain.
- Inflammatory Back Pain: Rheumatoid arthritis, ankylosing spondylitis and other spondyloarthropathies.
- Infections: Discitis, osteomyelitis, and spinal tuberculosis.
- Malignancies: Primary or metastatic cancers, including multiple myeloma.
- Visceral Causes: Referred pain from abdominal aortic aneurysms, renal calculi, or pancreatitis.
5. Symptoms
Back pain symptoms vary widely, but common presentations include:
- Localised Pain: May worsen with certain movements or prolonged positions.
- Radiating Pain: Pain that spreads to the legs or gluteal region, often indicative of nerve involvement (e.g. sciatica).
- Stiffness and Limited Mobility: Commonly seen in degenerative or inflammatory conditions.
- Neurological Deficits: Symptoms like numbness, tingling, weakness or loss of bladder/bowel control suggests possible spinal cord nerve compression, or cauda equina syndrome. These are neurosurgical emergencies.
6. Diagnosis
Diagnosis of back pain requires a comprehensive history and physical examination:
- Pain Characteristics: Assess location, onset, duration, radiation, and factors affecting the pain.
- Functional Assessment: Evaluation of posture, movement, and range of motion.
- Identification of Red Flags: Key signs indicating potential serious underlying pathology, such as fever, unintentional weight loss, history of cancer
- Progressive neurological deficits: Necessitate rapid investigation (MRI and neurosurgical opinion today).
Investigation
Imaging and additional diagnostic tests should be used selectively:
- MRI: Gold standard for assessing soft tissue structures, including intervertebral discs and nerve roots, especially in cases with neurological symptoms.
- CT Scans: Useful in some cases, particularly in complex fractures.
- Blood Tests: Full blood count, CRP, U+E, LFT, glucose and bone biochemistry (including calcium levels).
- X-rays: Limited use.
7. Treatment
Effective treatment strategies for back pain integrate pharmacologic, non-pharmacologic, and surgical options as appropriate:
- Conservative Therapy: Recommended as first-line treatment, including NSAIDs, paracetamol, and topical analgesics.
- Physical Therapy: Core strengthening, stretching, and mobility exercises are crucial for improving function and reducing recurrence risk.
- Pharmacologic Options: NSAIDs are commonly used; muscle relaxants and short-term opioid use may be considered for severe acute pain. Antidepressants or gabapentin etc are helpful in managing chronic neuropathic pain.
- Interventional Procedures: Epidural steroid injections, nerve blocks, or radiofrequency ablation may benefit patients with chronic pain who do not respond to conservative measures.
- Surgical Interventions: Reserved for severe cases, such as herniated discs causing significant neurological impairment, spinal stenosis, or instability.
8. Complications
Untreated or poorly managed back pain can lead to:
- Chronic Pain and Disability: Failure to resolve acute pain may result in long-term disability.
- Mental Health Impacts: Anxiety and depression are common comorbidities, especially with chronic pain.
- Reduced Quality of Life and Employment Impact: Persistent pain affects daily functioning, social engagement, and job performance, contributing to economic loss and reduced personal well-being.
9. Prognosis
- The prognosis for back pain depends on factors such as the underlying cause, the presence of psychosocial contributors, and adherence to treatment.
- Most cases of acute back pain resolve within six weeks, but chronic pain can persist, particularly in cases with comorbid mental health issues.
- Early intervention, including psychological support, often improves long-term outcomes and quality of life.
10. Prevention
Prevention strategies for back pain emphasize lifestyle changes and ergonomics:
- Exercise: Regular physical activity, including core strengthening, can help prevent back pain.
- Ergonomics: Proper workstation setup and adherence to safe lifting techniques are essential for those in physically demanding jobs.
- Weight Management and Smoking Cessation: Weight reduction and smoking cessation can reduce risk, particularly for degenerative disc disease.
- Education and Self-Management: Educating patients on posture, back care, and injury prevention can empower individuals to take control of their back health.
Summary
We have described 10 facts about back pain. We hope it has been helpful.
Other resource
Back Care UK is a national back pain charity.

