10 facts about haemorrhoids
Piles are very common and do not always need treatment. They normally affect adults and present as blood on the toilet paper when you wipe your bottom after a poo. They are not normally painful. If they are a problem, you can start with going to your local pharmacist for advice.
We will now describe 10 facts about haemorrhoids (piles).
Key Points
- Haemorrhoids, or piles, are swollen veins in the lower rectum or anus. They can occur internally or externally. They can cause discomfort, pain, and rectal bleeding. .
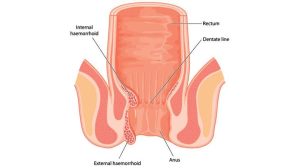
- They are classified as internal or external based on their location relative to the dentate line.
- Common risk factors include constipation, pregnancy, and prolonged straining.
- Diagnosis is usually clinical but may require additional investigation in cases of atypical symptoms.
- Treatment ranges from conservative management to surgical intervention depending on severity.
1. Definition
- Haemorrhoids are vascular structures within the anal canal, normally functioning to assist with stool control. When these veins become engorged and symptomatic, they are termed haemorrhoids or piles.
- Haemorrhoids are classified as internal (above the dentate line) or external (below the dentate line). Internal haemorrhoids may further be graded I-IV based on prolapse severity.
2. Epidemiology
- Haemorrhoids are common, affecting up to 50% of the UK population at some point in their lives, particularly those aged 45-65. However, the condition can occur at any age and affects both genders.
- Around 5% of individuals will seek medical treatment, and haemorrhoids are a frequent presentation in primary care and A&E.
3. Risk Factors
Several factors can increase the risk of developing haemorrhoids:
- Age: Prevalence increases with age due to weakening supporting tissues.
- Chronic constipation or diarrhoea: Both conditions lead to increased straining, impacting rectal blood flow.
- Pregnancy: Increased intra-abdominal pressure and hormonal changes contribute to haemorrhoid development.
- Obesity: Excess weight increases pelvic floor pressure.
- Dietary habits: Low-fiber diets can lead to constipation and straining.
- Prolonged sitting: Occupations that require prolonged sitting (e.g., desk jobs) can elevate rectal pressure.
- Genetic predisposition: A family history may increase the likelihood of haemorrhoid development.
4. Causes
- Haemorrhoids are caused by the distension and weakening of blood vessels in the anal canal, often due to increased venous pressure and weakened supportive tissue in the rectum.
- Straining from constipation or lifting heavy objects can exacerbate these conditions.
- Pregnancy-induced hormonal changes and physical pressure are also key contributors in women.
5. Symptoms
The clinical presentation of haemorrhoids varies based on their classification:
- Internal haemorrhoids: Typically present with painless rectal bleeding, seen as bright red blood on toilet paper or in the bowl. Symptoms may include pruritus, mucus discharge, and sensation of incomplete evacuation.
- External haemorrhoids: Often cause pain, especially if thrombosed. Patients may feel a palpable lump around the anus, accompanied by itching and discomfort.
- Prolapsed haemorrhoids: Grade III and IV internal haemorrhoids can protrude from the anal canal, causing significant discomfort.
6. Diagnosis
Diagnosis is primarily clinical, based on history and physical examination. Key steps include:
- History: Focus on bowel habits, bleeding patterns, and any family history of colorectal diseases.
- Physical Examination: Performed with the patient in the left lateral position. For external haemorrhoids, inspection may reveal visible lumps or swelling. For internal haemorrhoids, a digital rectal examination (DRE) and anoscopy/proctoscopy are often necessary to assess the location and grade of haemorrhoids.
Investigation
While haemorrhoids are often diagnosed clinically, further investigation may be warranted in specific cases:
- Anoscopy/Proctoscopy: Provides direct visualisation of internal haemorrhoids.
- Flexible Sigmoidoscopy/Colonoscopy: Indicated for patients with atypical bleeding, age over 40, or those with risk factors for colorectal malignancy.
- Complete Blood Count (CBC): To assess for anemia in cases of significant bleeding.
Differential Diagnosis
Conditions that can mimic haemorrhoid symptoms include:
- Anal fissures: Often painful, with bleeding associated with bowel movements.
- Anal fistula: Presents with chronic discharge and possible palpable tract.
- Colorectal carcinoma: Consider in patients over 40 with rectal bleeding or those with family history.
- Rectal prolapse: May present with a mass that protrudes through the anus but involves more of the rectal wall.
- Inflammatory bowel disease (IBD): Particularly with bleeding and tenesmus.
7. Treatment
Treatment of haemorrhoids varies according to symptom severity and haemorrhoid grade:
- Conservative Treatment: Recommended for early-stage haemorrhoids, includes:
- Dietary Modifications: High-fiber diet and adequate hydration to reduce constipation.
- Topical Treatments: Topical anaesthetics and corticosteroids can relieve symptoms temporarily.
- Warm Baths: Sitz baths help soothe perianal discomfort.
- Minimally Invasive Procedures: For symptomatic Grade II and III haemorrhoids:
- Rubber Band Ligation: Common for internal haemorrhoids; applies a band around the base to cut off blood supply.
- Sclerotherapy: Involves injection of a sclerosant to shrink haemorrhoids.
- Infrared Coagulation: Coagulates blood vessels, reducing haemorrhoid size.
- Surgical Intervention: Considered for Grade III-IV haemorrhoids or those unresponsive to other treatments.
- Haemorrhoidectomy: Complete excision, typically reserved for large or prolapsed haemorrhoids.
- Stapled Haemorrhoidopexy: Involves repositioning prolapsed tissue and cutting off blood supply.
8. Complications
Untreated haemorrhoids can lead to several complications:
- Anaemia: Chronic blood loss may result in iron-deficiency anaemia.
- Thrombosis: External haemorrhoids can thrombose, causing severe pain.
- Strangulation: Prolapsed haemorrhoids may become strangulated, leading to ischemia and gangrene.
- Infection: Rare, but infected haemorrhoids can cause abscesses and systemic infection.
9. Prognosis
- Most patients experience symptom relief with conservative management, especially if lifestyle changes are adhered to.
- However, haemorrhoids can be recurrent, particularly if risk factors persist.
- Advanced cases requiring surgery often have good outcomes, though recovery may involve discomfort.
1o. Prevention
Preventative strategies focus on maintaining good bowel habits to avoid straining:
- High-Fibre Diet: Aim for 20-30 grams per day.
- Adequate Hydration: Ensures softer stools.
- Regular Physical Activity: Helps prevent constipation.
- Avoiding Prolonged Straining: Encourage regular, prompt bowel movements without straining.
- Weight Management: Reduces intra-abdominal pressure.
- Avoiding Prolonged Sitting: Reduces pressure on rectal veins, especially during bowel movements.
When should I see a doctor about haemorrhoids?
It is recommended to see a doctor if you experience symptoms of piles, and:
- Bleeding between bowel movements
- Pain or discomfort
- Swelling or inflammation around the anus
- Itching or irritation around the anus
- A lump or bump near the anus.
Additionally, if you have a family history of colon cancer or if you are over the age of 50 years, it’s recommended to have a colonoscopy to rule out any other potential health concerns.
Summary
We have described 10 haemorrhoid facts. We hope you understand them better now.

