10 fibroid facts
In this article we will describe 10 fibroid facts: and focus on why there are problems with their diagnosis and treatment.
Key Points (and why there are problems)
-
Definition: are very common benign tumours of the uterus (womb); upto 7 in 10 White women and 8 in 10 Black women have one or more fibroids by age 50 years. As fibroids and (normal variant) heavy periods are so common, there is huge overlap; and confusion on whether either state is a disease,
-
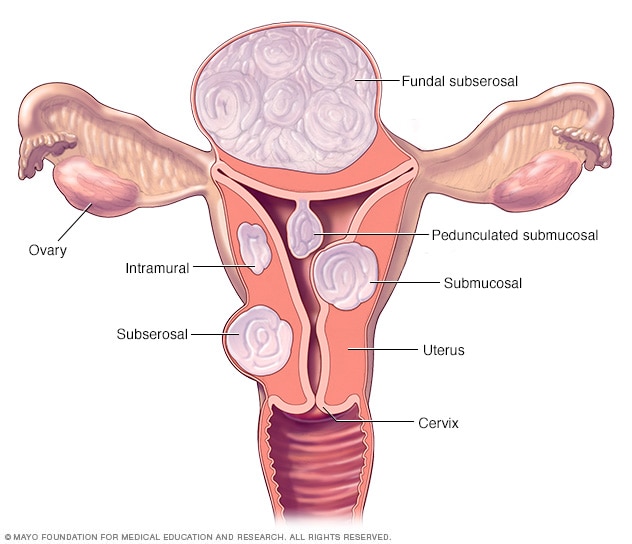
Types: include intramural, submucosal, subserosal, pedunculated, and intracavity. Treatment will not be the same for different types.
-
Symptoms: include heavy menstrual periods (commonest), pelvic pain, and infertility. We often do not like to talk about periods, delaying the diagnosis and treatment.
- Diagnosis: involves ultrasound, MRI, and histopathological examination (biopsy). None are 100% reliable.
-
Treatment: options range from conservative management to surgical intervention (embolisation or fibroid/uterus (womb) removal). It is not clear which is best and which is best for you. And they can recur after treatment.
- Natural history. They often regress (go away) with no treatment, e.g. after a pregnancy or menopause.
Note. The high prevalence means fibroids in most women are actually normal, not a disease, and usually don’t cause symptoms.
1. Definition
- Uterine fibroids, also known as leiomyomas, are (usually) non-cancerous tumours originating from the smooth muscle layer of the uterus. There is often more than one.
- They are composed of muscle and fibrous tissue.
- They are benign in more than 99% of cases and do not increase the risk for uterine cancer.
Types
-
Intramural fibroids: Grow within the uterine wall.
-
Submucosal fibroids: Project into the uterine cavity.
-
Subserosal fibroids: Grow outward from the uterus into the pelvis.
-
Pedunculated fibroids: Attach to the uterus by a stalk.
-
Intracavity fibroids: Grow within the uterine cavity.
Note. Fibroids may be tiny or as big as a football.
2. Epidemiology (who gets them)
-
Prevalence: 70-80% of women over 50 years have fibroids (yes, alot alot).
-
Peak incidence (of onset): Women aged 30 to 50 years.
-
More common: Black women.
Note. As they are so common, and having (normal variant) heavy periods is so common, it is hard to say that fibroids are the cause, i.e. know for certain that treatment will get rid of the symptoms.
3. Risk factors
-
Family history: First-degree relatives.
-
Obesity: Increased risk with higher BMI.
-
Early menarche: <12 years.
-
Black ethnicity: Higher incidence.
-
Nulliparity (not having had a baby): Increased risk.
4. Causes
-
Hormonal influences: Oestrogen and progesterone stimulate growth.
-
Genetic predisposition: Mutations in tumour suppressor genes.
5. Symptoms
-
Heavy menstrual periods (menorrhagia). This is the commonest presentation.
-
Prolonged menstrual periods.
-
Pelvic pain (pelvic pressure, discomfort).
-
Infertility or recurrent miscarriages.
-
Urinary frequency or constipation.
-
Abdominal swelling or bloating.
6. Diagnosis
-
Clinical evaluation: History, physical examination.
-
Imaging: Ultrasound (transvaginal or abdominal), MRI.
-
Histopathological examination: Biopsy or surgical specimen (removing a piece of the uterus/suspected fibroid).
Investigation
-
Ultrasound: Initial imaging modality.
-
MRI: Provides detailed anatomy.
-
Hysteroscopy: Key hole surgery to look inside the uterine cavity.
-
Laparoscopy: Evaluates pelvic organs.
Differential diagnosis
-
Adenomyosis.
-
Endometriosis.
-
Ovarian cysts
-
Pelvic inflammatory disease (PID).
-
Uterine polyps.
Problems with diagnoses
- Fibroids overlap with ‘normal heavy periods’ – i.e. and neither may be a disease.
- We don’t like to talk about periods.
- There is difficulty distinguishing fibroids from other conditions: (e.g. adenomyosis, endometriosis) due to overlapping symptoms and imaging limitations.
- Variability in presentation: Fibroids can be asymptomatic or cause severe symptoms.
7. Treatment
Treatment is difficult and complicated, as there are many options, each with pros and cons. This is partly why the condition is difficult for women (and their doctors) – not just the unpleasant symptoms that need to be controlled.
There is also a wide range of treatment for fibroids: from no treatment at all to surgery. Treatment is usually not necessary unless fibroids are causing excessive bleeding, pain, or bladder or bowel problems.
-
Conservative management: Watchful waiting, pain management.
-
Medical therapy: Hormonal treatments (e.g. GnRH agonists: leuprorelin (brand name Lupron) and triptorelin (brand name Decapeptyl).
-
Surgical options:
-
Myomectomy (operation to remove the fibroid(s)).
-
Hysterectomy (operation to remove the uterus).
-
Uterine artery embolisation (UAE). This means an x-ray technique to block off the blood supply to the fibroid(s).
-
Magnetic resonance-guided focused ultrasound surgery.
-
-
Minimally invasive procedures: Endometrial ablation, uterine fibroid embolisation.
Note. Natural history: fibroids often regress (go away) with no treatment, e.g. after a pregnancy or menopause. So it can be best to do nothing (conservative care).
When to see a doctor with possible fibroids
-
Heavy or prolonged menstrual periods.
-
Severe pelvic pain.
-
Infertility or recurrent miscarriages.
-
Abdominal swelling or bloating.
-
Urinary frequency or constipation.
8. Complications
-
Anaemia: Iron deficiency due to heavy bleeding,
- Problems getting pregnant (infertility) – with fibroids obstructing fallopian tubes.
- Miscarriage (when your pregnancy ends before 20 weeks).
- Going into labour too early.
- Unusual position of baby in the uterus.
- Postpartum haemorrhage (too much blood lost after birth).
Note. Fibroids can grow so big they can’t get enough blood. This makes them shrink and causes pain.
9. Prognosis
-
Most fibroids regress after menopause (or when pregnancy over). This is a issue with treatment as well. As they may ‘go away’ if you wait long enough.
-
Symptoms (usually) improve with treatment.
-
Recurrence possible after surgical interventions (they can come back). This is another issue, i.e. ‘definitive’ treatment is not perfect.
10. Prevention
-
Maintain healthy weight: Reduce risk.
-
Exercise regularly: Lower oestrogen levels.
-
Dietary modifications: Increase fibre, reduce red meat.
-
Stress management: Yoga, meditation.
-
Regular check-ups: Early detection and treatment.
Summary
We have described 10 facts about fibroids, and focused on why there are problems with diagnosis and treatment. There is a wide range of treatment for fibroids: from no treatment at all to surgery. We hope it has been helpful.
Other resources
- Uterine artery embolisation (UAE; 3rd edition). Royal College of Obstetricians and Gynaecologists (RCOG).
-
Heavy Menstrual Bleeding (2021). National Institute for Health and Care Excellence (NICE).
-
Uterine Fibroids (2020). American College of Obstetricians and Gynecologists (ACOG).

