10 myocardial infarction facts
In this article we will describe 10 medical revision notes on myocardial infarction (MI).
Key Points
- Myocardial infarction (MI), or heart attack, occurs when blood flow to a part of the heart muscle is blocked, usually by a blood clot that forms in a coronary artery – resulting in ischaemia and tissue necrosis
- ST-elevation myocardial infarction (STEMI) and non-ST-elevation myocardial infarction (NSTEMI) are the two main subtypes
- Prompt diagnosis and reperfusion therapy are crucial to reduce mortality and improve outcomes
- Risk factors include smoking, hypertension, diabetes, and family history of coronary artery disease
- Management includes reperfusion therapy (PCI or thrombolysis), medical therapy (antiplatelets, statins, ACE inhibitors), and lifestyle modification to prevent recurrence.
1. Definition
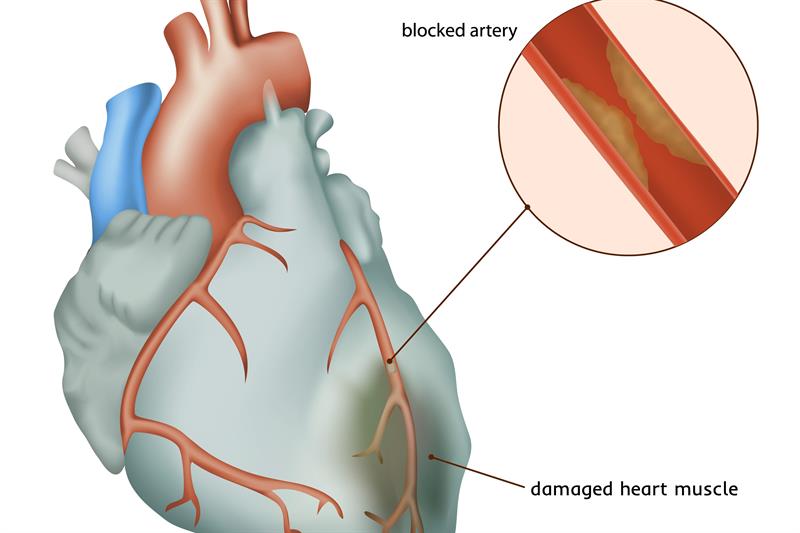
Myocardial infarction (MI), commonly referred to as a heart attack, occurs when blood flow to a portion of the heart is blocked, leading to ischemia and death of myocardial tissue. The blockage is usually due to a ruptured atherosclerotic plaque in a coronary artery, followed by thrombosis. There are two primary types:
- ST-elevation myocardial infarction (STEMI): Characterised by full-thickness necrosis of the myocardial wall and ST-segment elevation on ECG
- Non-ST-elevation myocardial infarction (NSTEMI): Involves partial-thickness necrosis without ST-segment elevation.
2. Epidemiology
- Prevalence: MI is a leading cause of death worldwide. In the UK, approximately 100,000 hospital admissions occur each year due to MI
- Age: MI predominantly affects older adults, with the risk increasing significantly after age 45 in men and 55 in women
- Gender: Men are at higher risk of MI compared to women, although the risk increases in post-menopausal women
- Mortality: Despite declining mortality rates due to improved treatment, MI remains a major cause of death, with early mortality (~10%) highest within the first 30 days.
3. Risk factors
Several modifiable and non-modifiable factors increase the risk of MI:
Modifiable
- Smoking: The most significant modifiable risk factor
- Hypertension: Uncontrolled blood pressure damages the arteries over time
- Diabetes mellitus: Increases atherosclerosis and promotes thrombus formation
- Dyslipidaemia: High LDL and low HDL cholesterol contribute to atherosclerotic plaque development
- Obesity and physical inactivity
- Excessive alcohol consumption.
Non-modifiable
- Age: Risk increases with age, particularly >45 years in men and >55 years in women
- Gender: Men are more affected, although women’s risk rises after menopause
- Family history: A history of premature coronary artery disease in first-degree relatives increases risk.
4. Causes
The most common cause of myocardial infarction is coronary artery disease (CAD), which involves atherosclerotic plaque buildup in the coronary arteries. Plaque rupture leads to thrombosis and occlusion of the artery. Other less common causes include:
- Coronary artery spasm (Prinzmetal’s angina): Transient spasm of coronary arteries causing temporary blockage
- Coronary artery dissection: A rare condition where the arterial wall tears
- Embolism: Thrombus or debris from other parts of the body can travel and occlude coronary arteries
- Severe anaemia or hypoxia, which increases myocardial oxygen demand.
5. Symptoms
Classic symptoms of MI include:
- Chest pain: The hallmark symptom, described as a heavy, crushing, or squeezing sensation. It may radiate to the left arm, neck, jaw, or back. It is usually of rapid onset (not sudden)
- Shortness of breath: Often accompanying chest pain, especially in older adults
- Sweating (diaphoresis): Profuse, cold sweats
- Nausea and vomiting
- Palpitations or dizziness.
Note 1. In some cases, especially in elderly patients, women, or people with diabetes, MI may present with atypical symptoms such as fatigue, indigestion, or vague discomfort without classic chest pain.
Note 2. The presence of nausea, vomiting and sweating favour myocardial infarction rather than ischaemia (angina).
6. Diagnosis
The diagnosis of MI is based on a combination of classical clinical symptoms, ECG findings, and biomarkers.
- Symptoms of ischaemia (e.g. chest pain).
- Electrocardiographic changes
- ST-elevation in at least two contiguous leads for STEMI
- ST-depression, T-wave inversion, or no specific changes for NSTEMI.
- Elevated cardiac biomarkers
- Troponins: Troponin T or I are the most sensitive and specific markers of myocardial injury
- Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality on echocardiography or cardiac MRI.
Note. 2/3 of classical clinical symptoms, ECG findings, and biomarkers, are needed to make a diagnosis of an MI.
Investigation
Several investigations help confirm MI and guide treatment:
- Electrocardiogram (ECG):
- STEMI: ST-segment elevation in two contiguous leads
- NSTEMI: ST-depression, T-wave inversion, or normal ECG.
- Cardiac biomarkers:
- Troponin I or T: Elevated in both STEMI and NSTEMI
- Creatine kinase-MB (CK-MB): Less specific than troponins but still used.
- Chest X-ray: To rule out differential diagnoses such as aortic dissection or pneumothorax
- Echocardiography: Assesses wall motion abnormalities and ejection fraction
- Coronary angiography: Definitive test to identify the location and severity of coronary artery blockages
- Blood tests:
- Full blood count (FBC): To check for anaemia
- Lipid profile: To assess cardiovascular risk factors
- Renal function and electrolytes: Important before initiating some treatments.
Differential diagnosis
Conditions that can mimic MI include:
- Unstable angina: Similar to NSTEMI but without elevated troponins
- Aortic dissection: Sudden, severe chest pain radiating to the back
- Pulmonary embolism: May present with chest pain and dyspnoea
- Pericarditis: Characterised by pleuritic chest pain relieved by sitting forward
- Gastro-oesophageal reflux disease (GORD): Chest discomfort, typically post-prandial and associated with acid regurgitation.
7. Treatment
The management of MI depends on whether the patient has STEMI or NSTEMI but involves three core elements: reperfusion therapy, medical therapy, and long-term management.
STEMI
- Reperfusion therapy:
- Primary percutaneous coronary intervention (PCI): The preferred treatment, ideally within 120 minutes of first medical contact. It restores blood flow, and relieve symptoms. In some cases, surgery may be necessary to restore blood flow.
- Thrombolysis: If PCI is unavailable within the window period, intravenous thrombolytic agents (e.g., alteplase) can be administered (to dissolve the clot)
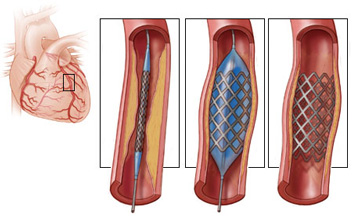 PCI for a heart attack
PCI for a heart attack
- Antiplatelet therapy:
- Aspirin: Administer 300 mg immediately
- P2Y12 inhibitor (e.g., clopidogrel, ticagrelor): To prevent further clot formation.
- Anticoagulation: Heparin or enoxaparin is given to prevent further thrombus formation.
NSTEMI
- Medical management:
- Dual antiplatelet therapy (DAPT) with aspirin and a P2Y12 inhibitor
- Anticoagulation with heparin or fondaparinux
- Beta-blockers: To reduce myocardial oxygen demand
- Nitrates: To relieve ischaemic pain
- Statins: Initiated early to stabilise plaques and reduce cholesterol levels.
- Risk stratification: Based on the GRACE score, early PCI may be indicated if the risk of further events is high.
Post-MI management
- ACE inhibitors (or ARBs) are used to reduce afterload and prevent adverse cardiac remodelling
- Statins to lower LDL cholesterol and prevent future cardiovascular events
- Lifestyle modifications including smoking cessation, weight loss, and regular exercise.
8. Complications
Complications of MI can be immediate or long-term:
- Cardiac arrhythmias: Ventricular fibrillation (VF), ventricular tachycardia (VT), or bradyarrhythmias
- Heart failure: Due to extensive myocardial damage
- Cardiogenic shock: A severe form of heart failure leading to multi-organ failure
- Pericarditis: Inflammation of the pericardium (Dressler’s syndrome occurs weeks after MI)
- Left ventricular aneurysm: Thinning and bulging of the infarcted wall
- Myocardial rupture: A rare but fatal complication of STEMI.
9. Prognosis
The prognosis of MI has improved significantly with modern treatments, but it depends on:
- Timeliness of reperfusion therapy: Prompt PCI or thrombolysis improves outcomes
- Extent of myocardial damage: Large MIs with reduced ejection fraction have a worse prognosis
- Comorbidities: Diabetes, hypertension, and heart failure increase mortality risk
- Post-MI care: Adherence to medications (statins, beta-blockers, ACE inhibitors) and lifestyle changes reduce the risk of recurrence.
In-hospital mortality is around 10% for STEMI, with higher rates in those with delayed reperfusion or severe comorbidities.
10. Prevention
Primary and secondary prevention of MI focuses on reducing modifiable risk factors:
Primary prevention
- Smoking cessation: The most significant risk factor for a first MI
- Control of hypertension and diabetes
- Lipid management: Statins for high-risk individuals
- Healthy diet: Low in saturated fat and refined sugars, rich in fruits, vegetables, and whole grains
- Regular exercise: At least 150 minutes of moderate-intensity aerobic activity per week.
Secondary prevention (post-MI)
- Dual antiplatelet therapy with aspirin and a P2Y12 inhibitor
- Beta-blockers, ACE inhibitors, and statins
- Cardiac rehabilitation: Supervised exercise and lifestyle modification programmes.
Summary
We have described 10 medical revision notes on myocardial infarction. We hope you understand it better now.
Top Tip
As the ECG may be normal initially in MI, do not send someone home with ischaemic sounding chest pain without senior review.
Other resource
MyHSN myocardial infarction podcast (2024) – 7 min, 32 sec

