Meningitis: Causes, Symptoms, Treatment
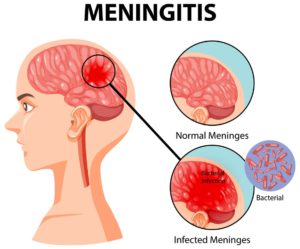
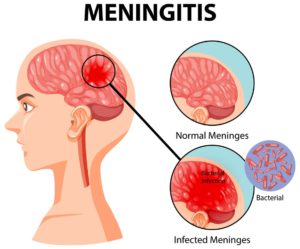
Diagram showing meningitis in human brain illustration
We will describe 10 facts for patients about meningitis.
Key Points
- Definition: meningitis is an inflammation of the meninges surrounding the brain and spinal cord, which can be life-threatening
- Microbiology: it can be caused by viral, bacterial, fungal, or parasitic infections, with bacterial meningitis being the most severe
- Treat as bacterial. Meningitis should be considered (and treated as) bacterial until otherwise proven
- Prompt diagnosis: and treatment are crucial to improve outcomes and reduce complications
- Vaccination and public health: measures play a significant role in prevention.
1. Definition
- Meningitis is defined as the inflammation of the meninges, the protective layers covering the brain and spinal cord
- This condition can lead to severe neurological complications and can occur at any age, although the aetiology (and organisms) varies with age.
2. Epidemiology
- Global incidence: Approximately 1.2 million cases of bacterial meningitis occur worldwide annually, with a higher prevalence in sub-Saharan Africa, particularly during epidemics in the ‘meningitis belt’
- Age distribution: Infants and young children are at the highest risk, but older adults (65+) and immunocompromised individuals are also vulnerable
- Outbreaks. Whilst rare, these can occur in close-contact settings such as schools or universities, military barracks, and day centres.
3. Risk factors
- Age: Infants, young children, and elderly adults are at higher risk
- Living conditions: Crowded settings (e.g. schools, military barracks) increase transmission, particularly for bacterial meningitis
- Immunocompromised status: Individuals with weakened immune systems (e.g., due to HIV, diabetes, or cancer) are more susceptible
- Recent infections: Upper respiratory infections or ear infections may precede bacterial meningitis
- Travel history: Certain geographic areas may have higher prevalence rates of specific meningitis pathogens.
4. Causes
Meningitis can be caused by various pathogens, including:
- Bacterial: Most common and severe forms are caused by Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae type b (Hib)
- Viral: Typically less severe; common viruses include enteroviruses, herpes simplex virus, and varicella zoster virus
- Fungal: Seen in immunocompromised patients, with Cryptococcus neoformans being a common causative agent
- Parasitic: Rare but can occur, particularly in endemic regions.
Transmission: For some organisms, droplet spread occurs requiring close contact. Meningitis can also result from direct spread (e.g. otitis media).
5. Symptoms
Symptoms of meningitis can develop rapidly and may include:
Classic triad
- Headache: Severe and persistent (gradual onset, compared to sudden with subarachnoid haemorrhage, SAH)
- Photophobia: Sensitivity to light
- Neck stiffness: Inability to flex the neck forward due to rigidity.
Other symptoms
- Fever: Often the first sign of infection
- Altered mental status: Confusion, lethargy, or difficulty concentrating
- Rash: A petechial or purpuric rash may indicate meningococcal meningitis
- Nausea and vomiting: Common accompanying symptoms.

A rash that does not fade under pressure can be a sign of ‘meningococcal septicaemia’. Meningococcal bacteria can cause meningitis and septicaemia (without meningitis).
6. Diagnosis
Diagnosis of meningitis involves a combination of clinical evaluation and laboratory testing:
- Clinical assessment: Obtain a thorough history and perform a physical examination, looking for signs of meningeal irritation (e.g., Kernig’s and Brudzinski’s signs)
- Lumbar puncture (LP): The gold standard for diagnosis, providing cerebrospinal fluid (CSF) for analysis
- CSF analysis: WC count, gram stain, glucose, protein, lactate, culture to determine the causative agent.
Investigation
Additional investigations may include:
- Blood cultures: To identify bacteria in the bloodstream
- Imaging studies: A CT scan or MRI may be performed before LP to rule out increased intracranial pressure or mass lesions if there are neurological deficits or altered consciousness
- Polymerase chain reaction (PCR): Used for rapid detection of viral pathogens in CSF
- Serological testing: May help identify specific viral or fungal infections.
Differential diagnosis
Three most important differential diagnoses
- Subarachnoid haemorrhage (SAH)
- Encephalitis (usually viral) – suggested by abnormal cerebral function, such as altered behaviour and speech or motor function, particularly if associated with fever
- Sepsis.
Other differential diagnoses
- Pneumonia, and other serious infections
- Central nervous system abscess
- HIV infection
- Other non-infective causes of meningitis, for example: Autoimmune disorders such as systemic lupus erythematosus (SLE, can cause aseptic meningitis) and Behçet’s syndrome.
7. Treatment
The treatment of meningitis varies based on the causative organism:
- Bacterial meningitis: Immediate intravenous (IV) antibiotics (e.g., ceftriaxone and vancomycin) and adjunctive corticosteroids to reduce inflammation
- Viral meningitis: Supportive care; antiviral medications may be required for specific viruses (e.g. IV acyclovir for herpes simplex virus, HSV)
- Fungal meningitis: Requires antifungal treatment, such as amphotericin B for cryptococcal infections
- Supportive care: Includes hydration, pain management, and monitoring for complications.
8. Complications
Complications of meningitis can be severe and may include:
- Sepsis: Bacterial meningitis can lead to septic shock
- Neurological deficits: Hearing loss, seizures, cognitive impairment, and motor deficits
- Hydrocephalus: Accumulation of CSF due to obstruction or impaired absorption
- Death: Particularly in untreated or severe cases of bacterial meningitis.
9. Prognosis
The prognosis for patients with meningitis depends on various factors:
- Causative organism: Significant mortality in bacterial meningitis (especially pneumococcal); viral meningitis generally self-limiting with good prognosis
- Timeliness of treatment: Early recognition and intervention improve outcomes
- Age and overall health: Younger and immunocompromised individuals may face worse outcomes.
10. Prevention
Preventive measures play a crucial role in reducing the incidence of meningitis:
- Vaccination: Immunisations against Haemophilus influenzae type b (Hib), Neisseria meningitidis, and Streptococcus pneumoniae are essential
- Prophylactic antibiotics: Close contacts of individuals with meningococcal meningitis may require prophylactic treatment (e.g. with ciprofloxacin or rifampicin)
- Public health measures: Education on the signs and symptoms of meningitis and promoting good hygiene practices.
Vaccination
The most effective way to prevent meningitis is through vaccination. There are vaccines available for bacterial meningitis caused by several different types of bacteria.
In the NHS, the ‘MenACWY’ vaccine offers protection against 4 types of bacteria that can cause meningitis: meningococcal groups A, C, W and Y.
The vaccine is offered to teenagers aged 14 years old. It is also offered to people up to the age of 25 who have never had a vaccine containing MenC.
Here is more information on NHS meningitis vaccination. Most are given in early childhood.
Summary
We have described 10 facts for patients about meningitis. We hope it has been helpful.
Top Tip – Meningitis
All patients with suspected meningitis should have a lumbar puncture usually after a CT head. You need to know the causative organism.