10 plantar fasciitis facts
5 Key Points
-
Plantar fasciitis affects 10% of adults, and is a common cause of heel pain in adults.
- It is characterised by inflammation of the plantar fascia, a band of tissue that supports the arch of the foot.
- Risk factors include age, obesity, and certain types of exercise.
- Diagnosis is typically made based on medical history and examination.
- Treatment options include conservative measures such as rest, stretching, and orthotics; as well as more invasive procedures like steroid injections and surgery.
In this article, we will describe 10 facts about plantar fasciitis.
1. Definition
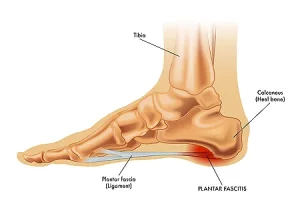
- Plantar fasciitis is a condition characterised by inflammation of the plantar fascia, a band of tissue that supports the arch of the foot.
- It is a common cause of heel pain in adults and can significantly impact daily activities and quality of life.
Types
There are two main types of plantar fasciitis:
-
Acute plantar fasciitis: This type is characterised by sudden onset of pain and inflammation.
-
Chronic plantar fasciitis: This type is characterised by persistent pain and inflammation that lasts for several months or years.
2. Epidemiology
Plantar fasciitis is a very common condition that affects approximately 10% of the adult population in the UK. It is more common in people aged 40-60 years and affects women more frequently than men.
3. Risk Factors
Several risk factors contribute to the development of plantar fasciitis, including:
-
Age: Plantar fasciitis is more common in people aged 40-60 years.
-
Obesity: Excess weight puts additional stress on the plantar fascia, increasing the risk of inflammation.
-
Exercise: Certain types of exercise, such as running, dancing, and jumping, can increase the risk of plantar fasciitis.
-
Foot mechanics: Abnormalities in foot mechanics, such as flat feet or high arches, can increase the risk of plantar fasciitis.
-
Occupation: People who work in jobs that involve standing or walking for long periods, such as nurses or teachers, are at increased risk of developing plantar fasciitis.
4. Causes
The exact cause of plantar fasciitis is not fully understood, but it is thought to be related to a combination of factors, including:
-
Overuse: Repetitive strain on the plantar fascia can lead to inflammation.
-
Trauma: Sudden injury to the plantar fascia can cause inflammation.
-
Biomechanical factors: Abnormalities in foot mechanics, such as flat feet or high arches, can increase the risk of plantar fasciitis.
5. Symptoms
The main symptom of plantar fasciitis is pain in the heel or bottom of the foot. The pain is often described as sharp or stabbing and can be worse in the morning or after periods of rest. Other symptoms and signs may include:
-
Tenderness: The heel or bottom of the foot may be tender to the touch.
-
Swelling: There may be swelling or redness in the affected area.
-
Limited mobility: Plantar fasciitis can cause stiffness or limited mobility in the foot or ankle.
Diagnosis
Diagnosis of plantar fasciitis is typically made based on medical history and examination.
- Medical history: To determine the onset and duration of symptoms, as well as any potential risk factors.
- Physical examination: To assess for tenderness, swelling, and limited mobility.
-
Imaging tests: Such as x-rays or ultrasound, to rule out other potential causes of heel pain. This is not usually necessary.
Investigation
In a few cases, imaging tests may be ordered to confirm the diagnosis and rule out other potential causes of heel pain. These may include:
-
X-rays: To rule out bone fractures or other bone-related conditions.
-
Ultrasound: To assess for inflammation or tears in the plantar fascia.
-
Magnetic Resonance Imaging (MRI): To provide detailed images of the plantar fascia and surrounding tissues.
Differential Diagnosis
The differential diagnosis for plantar fasciitis includes other potential causes of heel pain, such as:
-
Achilles tendonitis: Inflammation of the Achilles tendon.
-
Heel spur: A bony growth on the underside of the heel bone.
-
Stress fracture: A small crack in the bone.
7. Treatment
- Treatment for plantar fasciitis typically involves a combination of conservative measures and, in some cases, more invasive procedures.
- The goal of treatment is to reduce pain and inflammation, promote healing, and prevent future episodes.
Conservative Measures
-
Rest: Avoid activities that aggravate the condition.
-
Ice: Apply ice packs to the affected area for 15-20 minutes, several times a day.
-
Stretching: Perform calf and foot stretches to reduce tension on the plantar fascia.
-
Orthotics: Use shoe inserts or orthotics to support the arch and reduce stress on the plantar fascia.
-
Pain relief: Use over-the-counter pain medications such as paracetamol or ibuprofen.
More Invasive Procedures (not usually necessary)
-
Steroid injections: Inject steroids into the affected area to reduce inflammation.
-
Platelet-rich plasma (PRP) therapy: Inject platelet-rich plasma into the affected area to promote healing.
-
Surgery: In severe cases, surgery may be necessary to release the plantar fascia.
When to See a Doctor
It’s essential to seek medical attention if you experience any of the following:
-
Severe pain: If the pain is severe and interferes with your daily activities.
-
Persistent pain: If the pain persists or worsens over time.
-
Difficulty walking: If you have difficulty walking or standing due to pain.
-
Fever: If you have a fever in addition to heel pain.
-
Swollen heel: If the heel is swollen or red.
8. Complications
If left untreated, plantar fasciitis can lead to several complications, including:
-
Chronic pain: Plantar fasciitis can lead to chronic pain that persists for months or years.
-
Limited mobility: Plantar fasciitis can cause stiffness or limited mobility in the foot or ankle.
-
Heel spur: Plantar fasciitis can lead to the development of a heel spur, a bony growth on the underside of the heel bone.
-
Achilles tendonitis: Plantar fasciitis can increase the risk of developing Achilles tendonitis.
9. Prognosis
- The prognosis for plantar fasciitis is generally good, with most people experiencing significant improvement in symptoms with conservative treatment.
- However, some people may experience persistent or recurrent symptoms, and in severe cases, surgery may be necessary.
10. Prevention
Preventing plantar fasciitis involves taking steps to reduce stress on the plantar fascia, including:
-
Wearing supportive shoes: Wear shoes with good arch support and cushioning.
-
Stretching regularly: Perform calf and foot stretches regularly.
-
Maintaining a healthy weight: Excess weight can put additional stress on the plantar fascia.
-
Avoiding overexertion: Avoid activities that involve repetitive stress on the plantar fascia.
-
Using orthotics: Use shoe inserts or orthotics to support the arch and reduce stress on the plantar fascia.
Summary
We have describes 10 facts about plantar fasciitis. We hope it has been helpful.