This is how the AI article summary could look. Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat.
Prostate Cancer: Causes, Symptoms, Treatment
In this article we will describe 10 facts about prostate cancer.
5 Key Points
-
Most common cancer in men – with over 52,000 new cases in the UK diagnosed each year
- More common in older men – with 75% of cases diagnosed in men over 65 years
-
Majority of prostate cancers are slow-growing – and may not require immediate treatment.
- Early detection and diagnosis are critical – for effective treatment and improved patient outcomes
-
Treatment options for prostate cancer include surgery, radiotherapy, hormonal therapy, and active surveillance.
1. Definition
Prostate cancer is a malignant tumour that develops in the prostate gland; which is a small walnut-sized gland in men that produces seminal fluid. The prostate gland is located below the bladder and in front of the rectum.
-
Adenocarcinoma: Most common type, accounting for 90% of cases
-
Squamous cell carcinoma: Rare type that develops in the glandular cells
-
Small cell carcinoma: Rare and aggressive type
-
Neuroendocrine tumour: Rare tumour that develops in the neuroendocrine cells.
2. Epidemiology
- Prostate cancer is the most common cancer in men in the UK, with over 52,000 new cases diagnosed each year
- The incidence of prostate cancer increases with age, with 75% of cases diagnosed in men over 65 years
- Prostate cancer accounts for 13% of all cancer deaths in men in the UK.
3. Risk Factors
Several risk factors have been identified for prostate cancer, including:
-
Age: Prostate cancer is more common in older men
-
Family history: Men with a family history of prostate cancer are at increased risk
-
Genetic mutations: Certain genetic mutations, such as BRCA1 and BRCA2, increase the risk of prostate cancer
-
Ethnicity: Prostate cancer is more common in African and African-Caribbean men
-
Diet: A diet high in processed meat and low in fruits and vegetables may increase the risk of prostate cancer
-
Obesity: Obesity may increase the risk of prostate cancer.
4. Causes
The exact cause of prostate cancer is unknown, but several factors are thought to contribute to its development, including:
-
Genetic mutations: Genetic mutations can disrupt normal cell growth and division
-
Hormonal influences: Hormonal changes, such as an increase in testosterone, can stimulate the growth of prostate cells
-
Environmental factors: Exposure to environmental toxins, such as pesticides, may increase the risk of prostate cancer.
5. Symptoms and signs
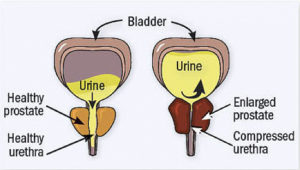
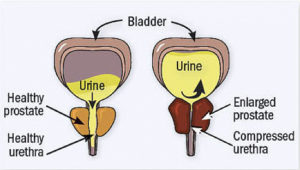
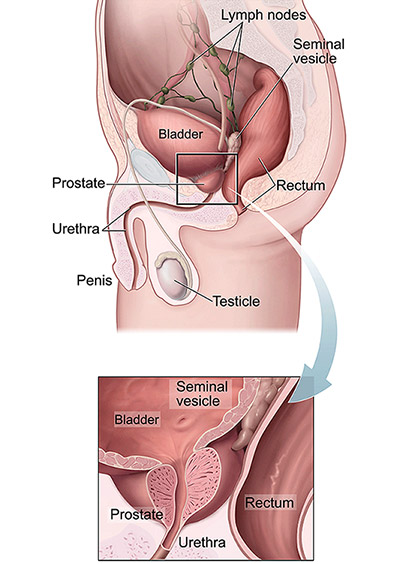 Location of prostate gland
Location of prostate gland
Symptoms
Prostate cancer often develops slowly and may not cause symptoms in the early stages. However, as the cancer grows, symptoms may develop, including:
-
Difficulty starting or stopping urination
-
Weak or interrupted flow of urine
-
Frequent urination, especially at night
-
Painful or burning urination
-
Painful ejaculation
-
Blood in the urine or semen
- Bone pain.
Signs
There may be no signs, especially in the early stages.
- Palpable bladder if in retention
- Firm prostate on DRE.
6. Diagnosis
Diagnosis of prostate cancer typically involves a combination of physical examination, laboratory tests, and imaging studies, including:
-
Digital rectal examination (DRE): A physical examination of the prostate gland
-
Prostate-specific antigen (PSA) test: A blood test that measures the level of PSA, a protein produced by the prostate gland
-
Transrectal ultrasound (TRUS): An imaging study that uses sound waves to create images of the prostate gland
-
Biopsy: A procedure in which a sample of tissue is removed from the prostate gland and examined under a microscope. A biopsy is the only way to know for sure if a tumour is cancerous.
Gleason Score
After a diagnosis of prostate cancer, a pathologist will determine a Gleason score for the tumour. Gleason scores are between 2 and 10 with less aggressive cancers in the 2-4 range and most aggressive in the 7-10 range.
Investigation
-
PSA test: A blood test that measures the level of PSA
-
PSA velocity: A measure of how quickly the PSA level is changing
-
PSA density: A measure of the PSA level per unit volume of the prostate gland
-
Imaging studies: Such as TRUS, MRI, or CT scans
-
Bone scan: A test that uses small amounts of radioactive material to detect cancer that has spread to the bones.
Differential Diagnosis
-
Benign prostatic hyperplasia (BPH): A non-cancerous enlargement of the prostate gland
-
Chronic Prostatitis: Inflammation of the prostate gland
-
Urinary tract infections (UTIs): Bacterial infections of the urinary tract.
7. Treatment
Treatment of prostate cancer depends on the stage and grade of the cancer, as well as the patient’s overall health. Treatment options include:
-
Surgery: Radical prostatectomy is the surgical removal of the prostate gland
-
Radiotherapy: External beam radiotherapy or brachytherapy may be used to treat prostate cancer
-
Hormone therapy: Hormone therapy may be used to reduce the levels of testosterone, which can help to slow the growth of prostate cancer
- Watchful waiting: Watchful waiting involves monitoring the cancer with regular PSA tests and digital rectal examinations, but without immediate treatment.
When to See a Doctor
Men should see a doctor if they experience any of the following symptoms:
-
Difficulty starting or stopping urination
-
Weak or interrupted flow of urine
-
Frequent urination, especially at night
-
Painful or burning urination
-
Painful ejaculation
-
Blood in the urine or semen
Men over 50 years should also discuss prostate cancer screening with their doctor.
8. Complications
-
Urinary incontinence: Prostate cancer and its treatment can cause urinary incontinence
-
Erectile dysfunction: Prostate cancer and its treatment can cause erectile dysfunction
-
Bone metastases: Prostate cancer can spread to the bones, causing bone pain and fractures
-
Spinal cord compression: Prostate cancer can spread to the spinal cord, causing spinal cord compression.
9. Prognosis
- The prognosis for prostate cancer depends on the stage and grade of the cancer, as well as the patient’s overall health
- Generally, the prognosis is good for men with early-stage prostate cancer, with a 5-year survival rate of over 90%.
Stage of prostate cancer
The stage of your cancer is one of the most important factors in choosing the best way to treat it. Prostate cancer is staged based on the extent of the cancer (using T, N, and M categories) and the PSA level and Gleason score (Grade Group) when it is first diagnosed.
10. Prevention
Unusually for a cancer, lifestyle choices may not increase your risk of prostate cancer.
Whilst there is no sure way to prevent prostate cancer, several lifestyle changes may help to reduce the risk, including: maintaining a healthy weight; eating a healthy diet; exercising regularly; avoiding smoking.
Bonus Fact
What is the prostate gland?
The prostate is a gland in the male reproductive system whose job is to produce the majority of fluid that protects and nourishes sperm cells in semen, the thick fluid that carries sperm. The prostate is only found in males.
It sits below the urinary bladder, in front of the rectum and surrounds the upper part of the urethra, the tube that carries urine from the bladder.
Prostate function is regulated by the male sex hormone testosterone.
The size of the prostate changes with age. It grows rapidly during puberty, fueled by the rise in male hormones (called androgens) in the body, such as testosterone and dihydrotestosterone (DHT).
Summary
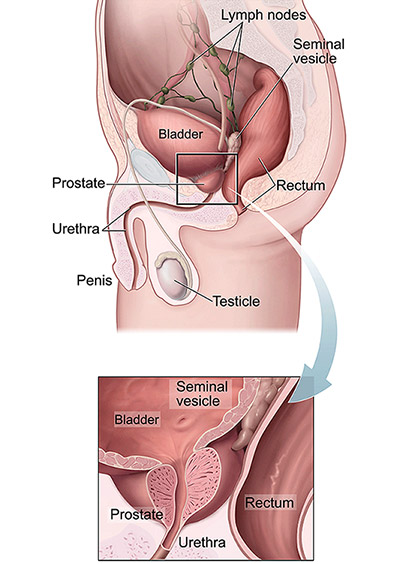 Location of prostate gland
Location of prostate gland