Skin Cancer: Causes, Symptoms, Treatment
Key Points
-
Skin cancer is the most common cancer in the UK, with over 100,000 new cases diagnosed annually
-
Incidence rates have increased by 45% in the past decade
- Three main types:
-
Melanoma: Most aggressive, deadliest, and accounts for most skin cancer-related deaths.
-
Squamous Cell Carcinoma (SCC): More aggressive, faster-growing, and may metastasise.
-
Basal Cell Carcinoma (BCC): Most common, slow-growing, and rarely metastasises.
-
Prevention is key. Early detection and treatment significantly improve prognosis. Skin cancer is highly treatable if detected early
-
Regular self-examination (and annual checks by a doctor if higher risk) can significantly improve prognosis.
1. Definition
- Skin cancer refers to the uncontrolled growth of abnormal cells in the skin. It is a malignant tumor that arises from the skin’s epithelial cells.
There are three main types of skin cancer:
-
Basal cell carcinoma (BCC): The most common type, accounting for approximately 75% of cases. Typically appears as a slow-growing, painless lump.
-
Squamous cell carcinoma (SCC): The second most common type, accounting for around 20% of cases. Often appears as a firm, pink or red lump.
-
Melanoma: The most aggressive and deadly type, accounting for around 5% of cases. Typically appears as a new or changing mole.
2. Epidemiology
-
Skin cancer is the most common cancer in the UK, with over 100,000 new cases diagnosed annually.
-
Incidence rates have increased by 45% in the past decade.
-
Men are more commonly affected than women.
3. Risk Factors
- Fair skin. People with blond or red hair and light-coloured eyes, and freckle or sunburn easily, are more likely to develop skin cancer than is a person with darker skin.
- Sun (UV light) effects:
- A history of sunburn. Having had one or more blistering sunburns as a child or teenager increases your risk of developing skin cancer as an adult. Sunburn in adulthood is also a risk factor.
- Excessive sun exposure. Anyone who spends considerable time in the sun may develop skin cancer, especially if the skin is not protected by sunscreen or clothing. Tanning, including exposure to tanning lamps and beds, also raises the risk. A tan is the skin’s injury response to excessive UV radiation.
- Sunny or high-altitude climate. People who live in sunny, warm climates are exposed to more sunlight than are people who live in colder climates. Living at higher elevations, where the sunlight is strongest, also increases exposure to more radiation.
- Moles. People who have many moles or abnormal moles called dysplastic naevi are at increased risk of skin cancer. These abnormal moles – which look irregular and are generally larger than normal moles – are more likely to become cancerous. If you have a history of abnormal moles, watch them regularly for changes.

Dysplastic naevi
- Precancerous skin lesions. Having skin lesions known as actinic (solar) keratoses can increase the risk of developing skin cancer. These precancerous skin growths typically appear as rough, scaly patches that range in colour from brown to dark pink. The are most common on the face, head and hands of fair-skinned people whose skin has been sun damaged.
- A family history of skin cancer. If a parents or sibling has had skin cancer, the patient may have an increased risk of the disease.
- A personal history of skin cancer. If the patient has developed a skin cancer once, they are at risk of developing it again.
- A weakened immune system. People with weakened immune systems have a greater risk of developing skin cancer. This includes people living with HIV/AIDS and those taking immunosuppressant drugs after an organ transplant.
- Exposure to radiation. People who received radiation treatment for skin conditions such as eczema and acne may have an increased risk of skin cancer, particularly basal cell carcinoma.
4. Causes
5. Symptoms
-
New or changing moles.
-
Unusual skin growths or lumps.
-
Bleeding or oozing from skin lesions.
-
Itching or pain in skin lesions.
Here is more about the three types.
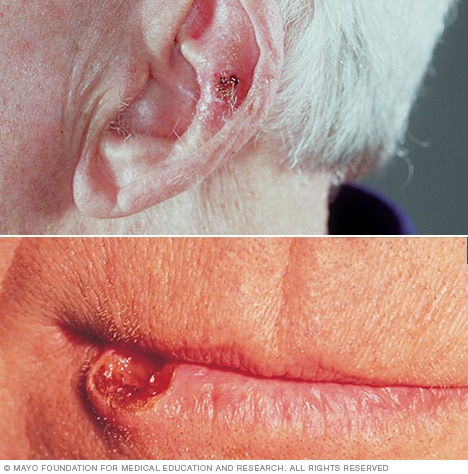
Basal cell carcinoma (BCC)

These usually occurs in sun-exposed areas of your body, especially on the face, near the eye, ear or nose.
Basal cell carcinoma may appear as:
- A pearly or waxy bump
- A flat, flesh-coloured or brown scar-like lesion
- A bleeding or scabbing sore that heals and returns.
Squamous cell carcinoma (SCC)
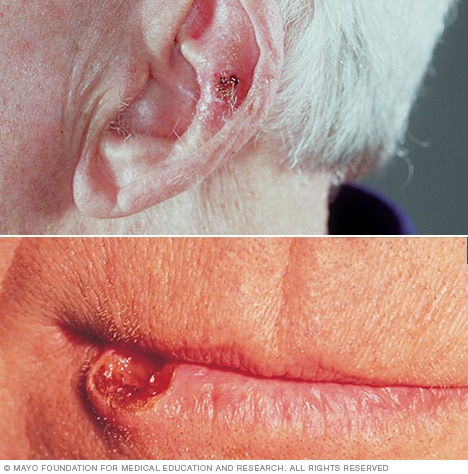
Most often, squamous cell carcinoma occurs on sun-exposed areas of your body, such as your face, ears and hands.
People with darker skin are more likely to develop squamous cell carcinoma on areas that are not often exposed to the sun.
Squamous cell carcinoma may appear as:
- A firm, red nodule
- A flat lesion with a scaly, crusted surface.
Melanoma

Melanoma signs include:
- A large brownish spot with darker speckles
- A mole that changes in colour, size or feel or that bleeds
- A small lesion with an irregular border and portions that appear red, pink, white, blue or blue-black
- A painful lesion that itches or burns
- Dark lesions on palms, soles, fingertips or toes, or on mucous membranes lining your mouth, nose, vagina or anus.
Melanoma can develop anywhere on your body, in otherwise normal skin or in an existing mole that becomes cancerous.
Melanoma most often appears on the face or the trunk of affected men. In women, this type of cancer most often develops on the lower legs.
In both men and women, melanoma can occur on skin that has not been exposed to the sun.
Melanoma can affect people of any skin tone. In people with darker skin tones, melanoma tends to occur on the palms or soles, or under the fingernails or toenails.
Investigation
Differential Diagnosis
-
Benign skin lesions (e.g. seborrheic keratoses, dermatofibromas).
-
Other skin cancers (e.g. Merkel cell carcinoma).
-
Inflammatory skin conditions (e.g. psoriasis, eczema).
7. Treatment
-
Surgery: Excision of the tumour with margins.
-
Topical treatments: Creams or gels for superficial BCC.
-
Radiotherapy: For inoperable or recurrent tumors.
-
Chemotherapy: For advanced or metastatic disease.
-
Immunotherapy: For melanoma.
When to see a doctor with a possible skin cancer
-
New or changing moles.
-
Unusual skin growths or lumps.
-
Bleeding or oozing from skin lesions.
-
Itching or pain in skin lesions.
8. Complications
-
Metastasis: Spread of cancer to lymph nodes or internal organs.
-
Recurrence: Return of cancer after treatment.
-
Disfigurement: Scarring or cosmetic deformity.
9. Prognosis
10. Prevention
-
Sun protection: Use sunscreen, clothing, and hats.
-
Avoid tanning beds.
-
Conduct regular skin self-examination.
-
Get vaccinated against HPV (human papillomavirus, which can increase skin cancer risk).
Summary
We have described 10 facts about skin cancer. We hope it has been helpful.