10 TB (tuberculosis) facts
In this article, we will describe 10 facts for health professionals about tuberculosis (TB).
Key Points
- Definition: TB is a contagious bacterial infection caused by Mycobacterium tuberculosis, primarily affecting the lungs but can involve any organ.
- Worldwide: TB remains a significant global health issue, with increased incidence in areas of poverty, overcrowding, and high HIV prevalence.
- Early diagnosis and completion of treatment: are essential to prevent transmission and the development of drug-resistant TB.
- Treatment: involves a prolonged course of multiple antibiotics, typically lasting at least six months.
- Prevention: include vaccination (BCG), prompt identification and treatment of active cases, and screening of high-risk groups.
1. Definition
- Tuberculosis is a chronic infectious disease caused by Mycobacterium tuberculosis#
- It primarily affects the lungs (pulmonary TB) but can also affect other parts of the body, including lymph nodes, bones, meninges, and kidneys (extrapulmonary TB)
- It spreads through airborne droplets when an infected person coughs, sneezes, or talks.
2. Epidemiology
- Global Burden: According to the World Health Organization (WHO), TB is one of the top 10 causes of death worldwide, with around 10 million new cases and 1.5 million deaths annually.
- UK Statistics: TB incidence in the UK has declined in recent years, with around 4,000 cases annually. However, the disease remains concentrated in certain urban areas, especially among specific high-risk populations.
- High-Risk Groups: Includes those with a history of travel to or residence in countries with high TB prevalence, people with HIV, those who are immunocompromised, and individuals living in crowded conditions.
3. Risk factors
- Close Contact with Infected Individuals: Especially in crowded or poorly ventilated settings.
- HIV Infection: Significantly increases the risk of progressing from latent TB infection (LTBI) to active TB disease.
- Immunosuppression: Due to conditions like diabetes, malnutrition, or use of immunosuppressive drugs (e.g. corticosteroids, TNF-alpha inhibitors).
- Living Conditions: Overcrowding, homelessness, and poor sanitation can contribute to increased TB transmission.
- Substance Use: Smoking, alcohol misuse, and intravenous drug use are associated with a higher risk of TB.
- Recent Travel: Exposure to high-prevalence regions, particularly sub-Saharan Africa, Southeast Asia, and Eastern Europe.
4. Causes
TB is caused by the bacterium Mycobacterium tuberculosis. It primarily spreads via:
- Inhalation of Airborne Droplets: When an infectious person coughs, sneezes, or talks, bacteria are released into the air and can be inhaled by others.
- Latent Infection: People can carry the bacteria without showing symptoms (latent TB). Approximately 5-10% of those with latent TB will develop active TB disease at some point, particularly if their immune system becomes weakened.
5. Symptoms
Pulmonary TB
- Persistent Cough: Lasting more than three weeks, often productive with sputum that may be blood-streaked (haemoptysis).
- Fever: Often low-grade, sometimes with night sweats.
- Weight Loss and Anorexia: Unexplained weight loss and reduced appetite are common.
- Fatigue and Malaise: Generalised weakness and lethargy.
Extrapulmonary TB
- Lymph Node TB (Tuberculous Lymphadenitis): Swollen, painless lymph nodes, often in the cervical region.
- TB Meningitis: Headache, altered mental status, neck stiffness, and neurological deficits.
- Skeletal TB: Localised pain and swelling, often in the spine (Pott’s disease).
- Genitourinary TB: Dysuria, haematuria, or flank pain.
- Disseminated (Miliary) TB: Can present with a range of systemic symptoms, including fever, night sweats, and organ-specific symptoms.
5. Diagnosis
Clinical diagnosis
- History and Examination: Consider TB in patients with persistent cough, systemic symptoms (fever, weight loss, night sweats), and risk factors. Physical examination may reveal signs such as lymphadenopathy or chest findings.
Investigation
- Chest X-Ray: Initial imaging for suspected pulmonary TB. Common findings include upper lobe infiltrates, cavitation, or pleural effusion. However, a normal chest X-ray does not rule out TB.
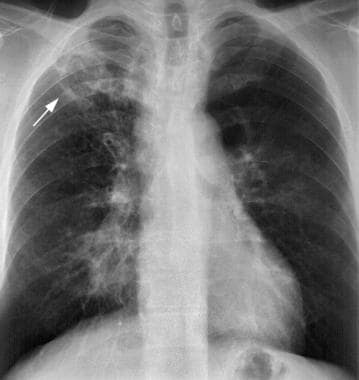
Typical TB on a chest x-ray
- Sputum Microscopy and Culture: Collection of three sputum samples (ideally early morning) for Ziehl-Neelsen stain (acid-fast bacilli). Sputum culture remains the gold standard for diagnosis but may take several weeks.
- Nucleic Acid Amplification Test (NAAT): Rapid diagnostic test for TB, including detection of drug resistance (e.g., GeneXpert).
- Mantoux Test (Tuberculin Skin Test): Screening test for latent TB. A positive result suggests prior exposure but does not confirm active disease.
- Interferon-Gamma Release Assays (IGRAs): Blood tests to detect latent TB infection, more specific than the Mantoux test and not affected by prior BCG vaccination.
- Extrapulmonary TB Investigations: May include biopsy, lumbar puncture, imaging (MRI, CT), and other site-specific tests, depending on the clinical presentation.
Differential diagnosis
- Pneumonia: Acute bacterial or viral infection of the lungs, presenting with cough, fever, and chest pain.
- Lung Cancer: Chronic cough, hemoptysis, and weight loss; often mimics TB, particularly in high-risk patients (e.g. smokers).
- Chronic Obstructive Pulmonary Disease (COPD): Chronic cough with sputum production, usually in smokers.
- Fungal Infections: Can present similarly, especially in immunocompromised patients (e.g. histoplasmosis, aspergillosis).
- Sarcoidosis: Granulomatous disease that may mimic TB on imaging but typically involves multiple organs.
7. Treatment
Anti-Tuberculous Therapy (ATT)
- First-Line Drugs: Standard treatment for drug-sensitive TB includes a combination of:
- Isoniazid (INH)
- Rifampicin (RIF)
- Ethambutol (EMB)
- Pyrazinamide (PZA)
- Treatment Regimen: The typical regimen is a 2-month intensive phase of four drugs (INH, RIF, EMB, PZA), followed by a 4-month continuation phase of two drugs (INH, RIF).
- Directly Observed Therapy (DOT): Recommended to ensure adherence, especially in patients at risk of non-compliance.
- Drug-Resistant TB: Multidrug-resistant TB (MDR-TB) requires longer treatment (18-24 months) with second-line drugs, such as fluoroquinolones and injectable agents. Extensively drug-resistant TB (XDR-TB) is even more challenging to treat.
Adjunctive Therapy
- Corticosteroids: May be used in certain cases, such as TB meningitis or pericarditis, to reduce inflammation and prevent complications.
- Nutritional Support: Important for recovery, particularly in malnourished patients.
8. Complications
- Drug-Resistant TB: Can develop due to incomplete or inappropriate treatment, requiring prolonged and more toxic drug regimens.
- Pleural Effusion and Empyema: Can occur in pulmonary TB.
- Chronic Pulmonary Damage: Cavities, bronchiectasis, and fibrosis may develop, leading to chronic respiratory symptoms.
- TB Meningitis: Can result in long-term neurological deficits, seizures, and hydrocephalus if not promptly treated.
- Miliary TB: Disseminated TB that can affect multiple organs, leading to severe systemic illness.
9. Prognosis
- Treatment Success: With appropriate treatment, most cases of drug-sensitive TB can be cured. Adherence to the full treatment course is essential to avoid relapse and resistance.
- Prognosis in Drug-Resistant TB: More challenging, with lower cure rates and increased risk of complications. Treatment is longer, more toxic, and less effective.
- Mortality: High in untreated cases, particularly in patients with HIV co-infection, drug-resistant TB, or disseminated disease.
10. Prevention
Primary Prevention
- BCG Vaccination: Given at birth in the UK to children at high risk of TB (e.g. with parents from high-prevalence countries). Provides some protection against severe forms of childhood TB (e.g. TB meningitis).
- Reducing Transmission: Prompt diagnosis and isolation of infectious cases, particularly in healthcare settings, to prevent spread.
Secondary Prevention
- Screening and Treatment of Latent TB: IGRAs or Mantoux tests in high-risk groups (e.g. healthcare workers, recent migrants from high-burden countries, immunocompromised individuals). Prophylactic treatment with isoniazid may be offered to prevent progression to active TB.
- Contact Tracing: Identifying and testing individuals who have been in close contact with active TB cases.
Summary
We have described 10 facts for health professionals about tuberculosis. We hope it has been helpful.
Other resource
MyHSN tuberculosis podcast (2024) – 7 min, 56 sec
Top Tip – Tuberculosis
If the patient is unwell (especially if from a high risk group), and TB is a possibility, treat it, whilst awaiting investigations.

