5 Stages of Diabetic Kidney Disease
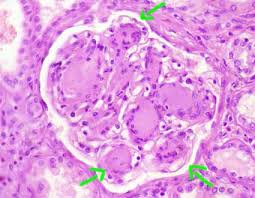
Establised diabetic nephropathy with Kimmelstiel-Wilson lesions arrowed.
In this article we will describe the 5 stages of Diabetic Kidney Disease – also known as diabetic nephropathy (DN). This is called the Mogensen classification of diabetic nephropathy. DN is a glomerular disease.
DN Stage 1. Hyperfiltration
- Years from diagnosis – at onset
- Dipstick – negative
- uACR – < 3 mg/mmol
- GFR – inc (>150 ml/min)
- Creatinine – N
- BP – N
- Renal biopsy – N (not usually done at any stage in diabetic nephropathy if clinical picture is clear)
- Renal ultrasound – N (not usually needed)
Treatment
There is no specific treatment for DN at this stage.
Stage 2. Normoalbuminuria (normal levels of proteinuria = protein in the urine)
- Years from diagnosis – 2-5 years
- Urine dipstick – negative
- uACR (urine lab test) – < 3 mg/mmol
- GFR – N (60-120 ml/min)
- Creatinine – N
- BP – N
- Renal biopsy – N
- Renal ultrasound – N (not usually needed)
Treatment
There is no specific treatment for DN at this stage. But tight control of blood pressure and glucose (maintaining stable blood sugar levels) can help slow the progression of diabetic nephropathy at this stage – and is part of the prevention strategy.
Stage 3. Microalbuminuria (higher levels of proteinuria)
- Years from diagnosis – 5-10 years
- Dipstick – N/positive
- uACR – 3-30 mg/mmol
- GFR – N (60-120 ml/min)
- Creatinine – N (60-120 mcmol/L)
- BP – N/+
- Renal biopsy – N (or glomerular basement membrane (GBM) thickening, and mesangial expansion)
- Renal ultrasound – N (not usually needed)
In the early stages, diabetic nephropathy often presents as microalbuminuria, which means there are small amounts of albumin (a protein) in the urine. This is an early sign of kidney damage and the patient will not notice any symptoms. This is why as soon as someone develops diabetes, they need regular testing of their urine for microalbuminuria (minimum is yearly).
Treatment
There continues to be no specific treatment for DN at this stage. But continued tight control of blood pressure (120/70 or less), glucose (maintaining stable blood sugar levels) and urinary protein may slow the progression of diabetic nephropathy at this stage as well.
Medication such as angiotensin-converting enzyme inhibitors (ACE, e.g. Ramipril) or angiotensin receptor blockers (ARBs, e.g. Losartan); and/or SGLT2 inhibitors (e.g. Dapagliflozin) should be prescribed. These help to reduce the protein levels in the urine, as well as control the BP.
Stage 4. Overt nephropathy/macroalbuminuria (higher levels of proteinuria)
- Years from diagnosis – 10-25 years
- Dipstick – positive
- uACR – >30 mg/mmol (often >100 mg/mmol)
- GFR – dec (15-60 ml/min)
- Creatinine – inc (120-400 mcmol/L)
- BP +
- Renal biopsy – nodular glomerulosclerosis (Kimmelstiel-Wilson lesions) +/- hypertensive changes
- Renal ultrasound – N
As the disease progresses, microalbuminuria can advance to macroalbuminuria, where larger amounts of albumin are excreted in the urine. This indicates more severe kidney damage.
High levels of protein in the urine is a hallmark of advancing DN, and is a serious sign. The urine may become frothy when it develops. When the protein levels in the urine are high enough, and blood protein levels are low enough, it is called ‘nephrotic syndrome’.
Regarding GFR, patients are usually in CKD3B-4 at this stage.
Treatment
Medication such as angiotensin-converting enzyme inhibitors (ACE, e.g. Ramipril) or angiotensin receptor blockers (ARBs, e.g. Losartan); and/or SGLT2 inhibitors (e.g. Dapagliflozin) should be prescribed. These help to reduce the protein levels in the urine.
Over time, in some patients, the kidneys’ ability to filter waste and excess fluid from the blood deteriorates. This leads to a worsening renal function and CKD, and increased urinary protein levels; resulting in symptoms such as fatigue, ankle swelling, shortness of breath (ankle and pulmonary oedema). Diuretics (water tablets) may be required at this stage.
Stage 5. ESRF (CKD5, i.e. kidney failure)
- Years from diagnosis – > 15 years
- Dipstick – positive
- uACR – >30 mg/mmol (often >100 mg/mmol)
- GFR – dec (<15 ml/min)
- Creatinine inc (> 400 mcmol/L)
- BP ++
- Renal biopsy – nodular glomerulosclerosis (Kimmelstiel-Wilson lesions) +/- hypertensive changes +/- chronic scarring
- Renal ultrasound – N (or small kidneys, or cortical thinning)
Treatment
Despite all interventions, patients with severe DN will need to be prepared for dialysis; plus or minus a kidney or kidney-pancreas (type 1 DM only) transplant.
PD may be preferred over HD as: a. many patients with DM have poor veins for a fistula; b. there is a concern re anticoagulation in HD worsening diabetic retinopathy.
The outlook on dialysis is not good, with an average survival of 3 years from the start of dialysis.
Who should look after these patients?
- Stage 1-3. GP
- Stage 4. Be seen by (or discussed with) kidney specialist (nephrologist)
- Stage 5. Nephrologist.
Summary
We have described the 5 stages of Diabetic Kidney Disease. We hope it has been helpful.

