Acute and chronic pancreatitis facts – patient information
In this article, we will describe 10 acute and chronic pancreatitis facts.
1. Definition
Pancreatitis is the inflammation of the pancreas, an organ located behind the stomach. It can be acute (short-term) or chronic (long-term).

2. Risk factors
These include: excessive alcohol consumption (people who consume 4-5 drinks a day), cigarette smoking. obesity, diabetes and a family history of pancreatitis.
The role of genetics is becoming increasingly recognised in chronic pancreatitis. If you have family members with the condition, your odds increase – especially when combined with other risk factors.
3. Cause
Acute pancreatitis. The most common cause of acute pancreatitis is gallstones, which can block the pancreatic duct and trigger inflammation. Other causes include alcohol use, certain medications, infections, and abdominal trauma.
Chronic pancreatitis. This is often caused by long-term alcohol use; although it can also result from recurring acute pancreatitis episodes, hereditary factors, cystic fibrosis, or certain autoimmune diseases.
4. Who gets it?
Acute pancreatitis. This is more common in middle-aged and elderly people, but it can affect people of any age. Men are more likely to develop alcohol-related pancreatitis; whilst women are more likely to develop it as a result of gallstones.
Chronic pancreatitis. In 30% of people chronic pancreatitis, the cause cannot be identified – this is known as ‘idiopathic’ chronic pancreatitis. Chronic pancreatitis can affect people of any age, but is most common in middle-aged men aged between 45-55 years.
5. Symptoms
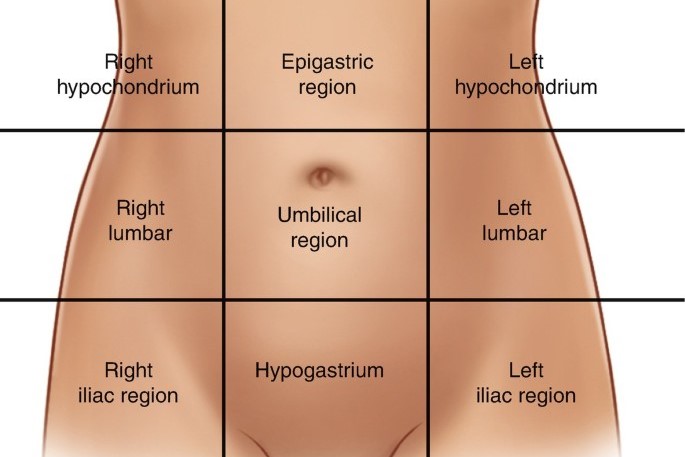
Acute pancreatitis usually presents with a rapid onset of severe abdominal pain (especially in the epigastrium) often radiating to the back; associated with nausea, vomiting, fever, and a rapid pulse.
In chronic pancreatitis, patients experience long-term abdominal pain, weight loss and oily, foul-smelling stools.
6. Complications
These can be serious and even life-threatening. They include pancreatic pseudocysts (fluid-filled sacs), infection, pancreatic necrosis (tissue death), abscess formation, diabetes mellitus, and pancreatic cancer in some cases.
7. Diagnosis
This involves a combination of medical history and examination, blood tests (e.g. amylase and lipase levels); imaging tests (such as ultrasound, CT scan, or MRI); and sometimes an endoscopic procedure (ERCP), to visualise the pancreas.
8. Treatment
Acute pancreatitis. This involves hospital admission, pain management, intravenous fluids, and fasting to give the pancreas time to heal. Delayed surgical intervention may be necessary to remove gallstones (cholecystectomy) or drain pseudocysts.
Chronic pancreatitis. This requires long-term management to relieve symptoms and prevent complications. Treatment often includes lifestyle modifications such as avoiding alcohol and adopting a low-fat diet, pancreatic enzyme replacement therapy, pain medication, and sometimes surgery.
9. Alcohol cessation
This is crucial in preventing or managing both types of pancreatitis, as continued alcohol abuse can worsen the condition and increase the risk of complications.
10. Recurrence
Acute pancreatitis can be a recurrent condition, particularly in chronic pancreatitis. Patients with a history of pancreatitis should work closely with their doctor to manage the condition; follow recommended dietary and lifestyle changes, and receive regular check-ups.
Summary
We have described 10 acute and chronic pancreatitis facts for patients. We hope it has been useful.

