Asthma – medical revision notes
We will describe 10 medical revision notes about asthma, focusing on its symptoms, causes, and treatment. Let’s start with the basics.
It is a chronic respiratory condition that affects the airways, making them inflamed and narrowed; leading to symptoms such as wheezing, coughing, chest tightness, and difficulty breathing.
Key Points
- Asthma is a chronic inflammatory disease of the airways that leads to airflow obstruction
- It is characterised by bronchial hyperreactivity and airway inflammation
- Early diagnosis and appropriate management are crucial to reduce morbidity and improve quality of life
- A multiprofessional approach, including patient education, medication adherence, and environmental control, is essential in managing asthma.
1. Definition
- Asthma is defined as a chronic respiratory condition characterised by recurrent episodes of wheezing, breathlessness, chest tightness, and coughing
- These symptoms are typically worse at night or early in the morning and are associated with widespread but variable airflow obstruction, which is often reversible either spontaneously or with treatment
- A key characteristic of asthma is that the airway narrowing is reversible, and the airways go back to normal between attacks. This makes it different from COPD where the airways may be tighter than normal all the time (and further tightened during attacks).
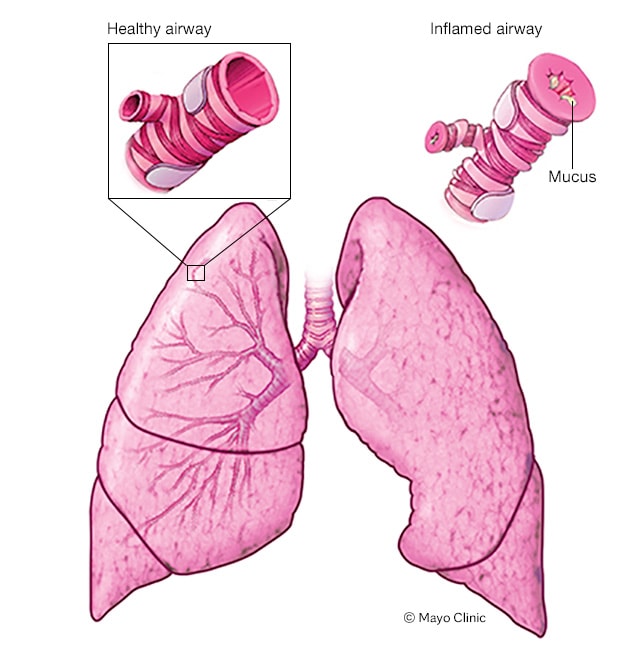
Airways in an asthma attack
2. Risk Factors
Asthma can affect individuals of all ages but is more commonly diagnosed in childhood.
- Genetic predisposition: Family history of asthma or atopic conditions (e.g. eczema, allergic rhinitis)
- Environmental factors: Exposure to allergens (pollen, dust mites, pets), tobacco smoke, air pollution, and occupational irritants
- Respiratory infections: Viral infections, especially in early childhood, can increase the risk
- Obesity: Increased body mass index (BMI) is linked to higher asthma prevalence and severity
- Physical activity: Exercise can trigger symptoms in some patients.
4. Causes
Asthma is primarily caused by a combination of genetic and environmental factors that lead to chronic inflammation of the airways. The following mechanisms contribute:
- Airway inflammation: Exposure to allergens or irritants triggers an inflammatory response
- Bronchial hyperresponsiveness: The airways become overly sensitive to stimuli, leading to excessive constriction
- Airway remodelling: Chronic inflammation can result in structural changes in the airway, including smooth muscle hypertrophy and collagen deposition.
5. Symptoms
- Wheezing: A high-pitched whistling sound during breathing, especially on exhalation
- Shortness of breath: Often occurs during physical activity or at night
- Chest tightness: A feeling of constriction or pressure in the chest
- Coughing: Typically worse at night or early morning, can be persistent or episodic.
6. Diagnosis
Diagnosis of asthma is primarily clinical but may involve the following:
- History taking: Assess for symptom patterns, triggers, and family history
- Physical examination: Look for signs of respiratory distress and listen for wheezing
- Spirometry: Measurement of lung function to assess airflow limitation; a reduced FEV1/FVC ratio that improves with bronchodilator use suggests asthma
- Peak expiratory flow (PEF) monitoring: Measures variability in airflow over time
- Bronchoprovocation testing: May be performed to assess bronchial hyperresponsiveness.
Investigations
Further investigations may include:
- Allergy testing: Skin prick tests or specific IgE blood tests to identify potential allergens.
- Exhaled nitric oxide (FeNO) testing: Measures airway inflammation.
- Chest X-ray: To rule out other conditions (e.g., infections, tumors) but is not diagnostic for asthma.
- Sputum analysis: To evaluate eosinophil levels in chronic asthma cases.
7. Treatment
Management of asthma includes both pharmacologic and non-pharmacologic strategies:
- Medication:
- Bronchodilators: Short-acting (SABAs) for quick relief and long-acting (LABAs) for control
- Anti-inflammatory agents: Inhaled corticosteroids (ICS) are the cornerstone of long-term management
- Leukotriene receptor antagonists (LTRAs): For patients with allergies or exercise-induced symptoms
- Biologics: Targeted therapies (e.g. omalizumab) for severe asthma cases.
- Patient education: Teach proper inhaler technique and the importance of adherence to medication
- Action plan: Develop an asthma action plan for self-management, including symptom monitoring and trigger avoidance.
8. Complications
- Severe asthma exacerbations: Can result in hospitalisation (including intensive care) or respiratory failure
- Chronic obstructive pulmonary disease (COPD): Long-term asthma can lead to irreversible airflow obstruction
- Psychosocial effects: Increased anxiety and depression due to chronic illness
- Reduced quality of life: Limitations in daily activities and exercise.
9. Prognosis
The prognosis for individuals with asthma varies widely based on several factors:
- Control of symptoms: Most patients can achieve good control with proper management
- Adherence to treatment: Consistent use of medications significantly improves outcomes
- Age at onset: Childhood asthma may resolve in some cases, but adult-onset asthma can be more persistent.
10. Prevention
- Avoidance of triggers: Identify and minimise exposure to allergens and irritants
- Regular monitoring: Use PEF measurements to track lung function
- Vaccinations: Influenza and pneumococcal vaccines to prevent respiratory infections
- Education and self-management: Empower patients with knowledge about their condition and action plans to prevent exacerbations.
Summary
We have described 10 medical revision notes about asthma, including its symptoms, causes, and treatment. We hope you understand it better now.

