How to be effectively discharged from hospital (5 steps) – and not readmitted
5 things need to be done to carry out an effective discharge – from your (and the hospital’s) point of view:
1. Medication
2. Discharge summary
3. Transport and preparing home
4. Follow-up
5. Feedback.
Remember. You have the right to discharge yourself from hospital at any time during your stay in hospital.
We will now go through how to be effectively discharged from hospital (5 steps) – and not readmitted. This is written from a patient’s point of view.
1. Medication
Ensure you do not leave hospital without the medication you need.
Ask to speak to a pharmacist before you leave to go through your new medication slowly.
If you are given any medication to take home, you’ll usually be given enough for the following 7 days. The letter to your GP (called a discharge summary) will include information about your medication (see below).
If you need to keep taking your medication, make sure you arrange to get a repeat prescription from your GP before your hospital supply runs out. Some surgeries require up to 2 working days (48 hours) notice for repeat prescriptions.
If you’re registered for patient online services with your GP, you could order your repeat prescription through the NHS app or their website.
Your local pharmacy can help you get on top of your new medicines.
Medical devices
If you’re sent home with a medical device (especially a new one), make sure you know how to set it up and have been taught how to use it.
Also, make sure you know where to get any supplies you need to use the device and who to call if you need help.
2. Discharge summary
Do not leave hospital without a copy of a letter called a discharge summary. As the name suggests its a summary of your stay. A good one will state:
- Where you were (ward)
- Your consultants name
- Date of arrival and discharge
- Diagnosis and treatment
- Medication (to go home with)
- Follow-up.
Make sure that it has either been emailed (or sent first class) to your GP. Keep a copy (ask for one, if not offered). Put that summary in your medical record (more info on that on MyHSN here). It is important.
Example
This is an example of a discharge summary template. All parts should be filled out.
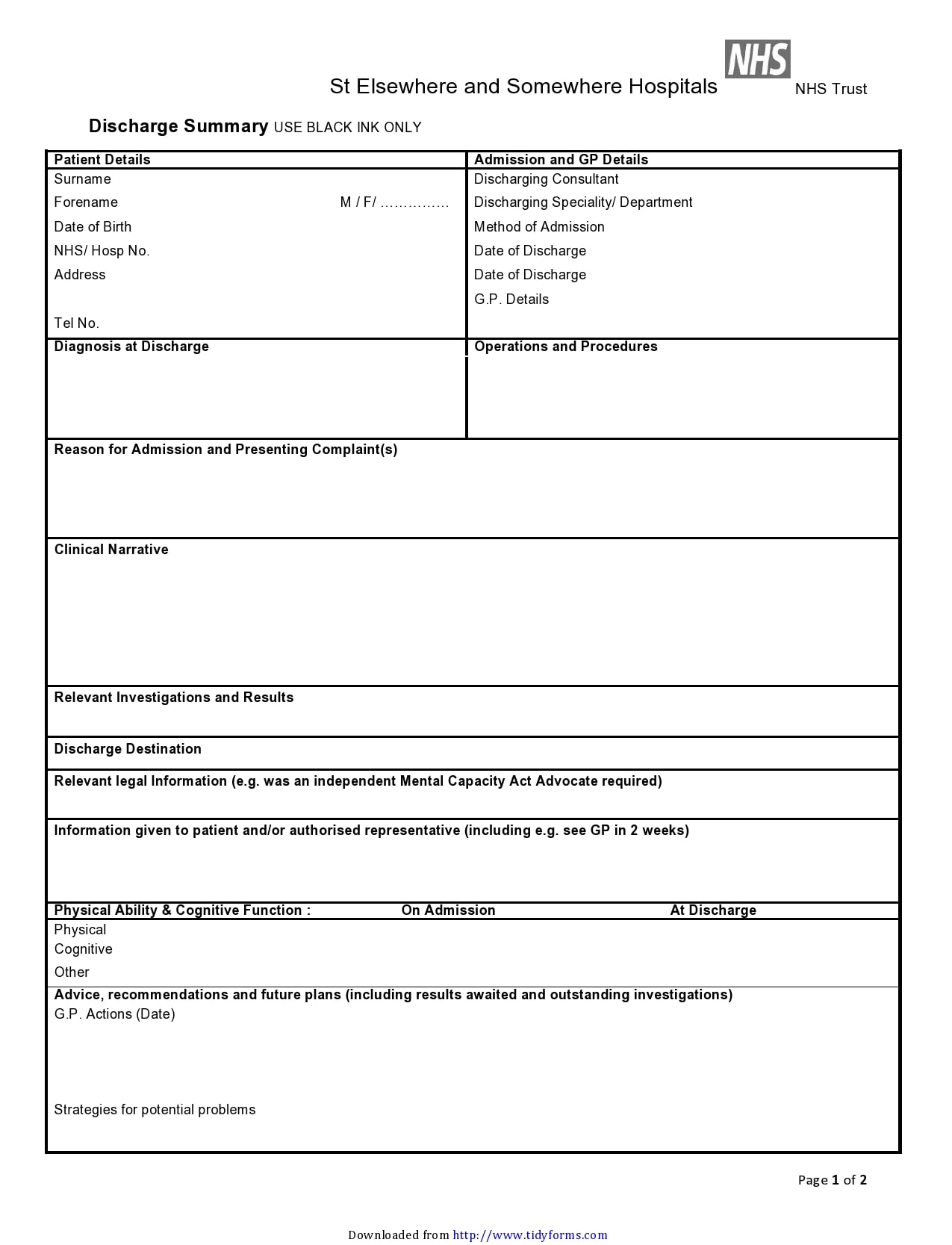 A typical discharge summary
A typical discharge summary
3. Transport and preparing home
Organising transport
If you’re being discharged, arrange for a relative or friend to collect you, or let the staff know if they need to make other transport arrangements for you.
Preparing home
If you’re returning home, make sure you have everything you need for your recovery. It may be helpful to ask a friend or relative to stay with you or visit regularly.
If this is not possible, make sure you have plenty of food, drink and other essentials at home.
Sick note
You may need a sick note or information for insurance companies or your employer. Speak to the nurse in charge of your ward, or ward clerk, if you need a form to be completed.
4. Follow-up
Most admissions will need follow-up, either
- With hospital consultant (and/or team): within 2 months of discharge (or within 2 weeks, if there is a key test result ‘in the air’ – i.e. not back yet))
- GP (you may have to organise, ideally about 2 weeks after discharge)
- Both.
Ask what are the exact hospital follow-up arrangements: Date/time? Where? With who? Who to ring if nothing happens? etc
5. Feedback
If you care has been good, feel free to leave a card and/or write a letter to the consultant, nurse in charge of the ward, or Chief Executive. We like positive feedback if we deserve it!
But. Also talk to nurses and doctors, and/or ward clerk, if you’re unhappy about your suggested discharge or transfer date.
Alternatively, speak to a PALS team member at the hospital. They will have an office near the main entrance. You can ask for a PALS staff member to come and talk to you. PALS offers confidential advice, support and information.
Some other stuff
- Make sure the hospital’s computer system is correct (and up-to-date) with your contact details, e.g. name, DoB, address, mobile and landline numbers, GP.
- Make sure you know the name of your consultant and their secretary’s phone number and email address.
Two types of discharge
Simple (80%)
The majority of discharges are simple and require the above 5 to be done, but not a lot more. You, with a little help, will be able to do most of the discharge yourself.
Complex (20%)
A smaller number are complex, usually for frail elderly patients. They require a lot of work from you, your family, carers and nursing/residential home. Make sure your family have been liaising with the hospitals’ social workers. Do not go home unless you think things are as sorted as they can be. For example, if your ‘care plan’ has been changed, has everyone involved been informed?
Summary
We have explained how to be effectively discharged from hospital (5 steps) – and not readmitted. The are the 5 things that need to be done for a patient to achieve a ‘good discharge’. If all these things are done, you should get home efficiently, and be well when you get there – and readmission should be prevented. Complex ones need careful planning to be successful.
Good follow-up, good communication, and correct medication, are the keys to avoiding readmission.


