10 back pain facts
We will describe how to relieve a sore back, as part of 10 facts about back pain.

Most back pain is usually multi-factorial, and may originate from any of the structures in and adjacent to the spine including: muscles, ligaments, bones (vertebrae), and the intervertebral discs (cushions which sit in between each of the vertebrae). Injury to any of these structures may precipitate an episode of acute back pain (an acute sore back).
1. So. How to relieve a sore back? Here are 5 things to do
- Medication – take anti-inflammatory (NSAID) medicine like aspirin or ibuprofen regularly (4x a day). Paracetamol can be used with another painkiller, taken at the same time as a NSAID
- Ice or heat – apply an ice pack or bag of frozen peas wrapped in a tea towel to reduce pain and swelling, especially immediately after an injury. After about 48 hours, you can try using a heating pad or hot water bottle wrapped in a tea towel to relieve muscle spasms or joint stiffness
- Movement – getting up and walking every hour can help alot. Try not to lie in bed. Longer term, gentle exercise like walking, swimming, cycling, yoga, or stretching can increase blood flow and promote healing. Strengthening your core muscles can also help
- Massage – can help with sore muscles and injury recovery by providing nutrients to tissues. It can also relieve tension knots in the back or shoulder muscles
- Distraction – try to distract yourself so your thoughts aren’t fixated on the pain. Getting a good night’s sleep can help with recovery. Using sleeping tablets in the short-term may help.
Here are 9 more facts, more concerning long-term back pain.
2. Back pain is normal. Most humans have or have had it. In fact, 80% of the population have it at some point in their lifetime. And it is responsible for 40% of all lost work days.
3. Prevention and treatment of long-term back pain
- Lose any excess weight – use a healthy weight calculator to find out if you’re a healthy weight for your height. Keep BMI under 30 if you can. This is the most useful thing you can do to help yourself
- Exercise – your back regularly. Walking, swimming (including front and back stroke) and using exercise bikes and cross-trainers, are all excellent ways to strengthen your back muscles. Running, particularly on hard surfaces and for long periods, is likely to exacerbate back pain. So finding a way of staying fit without repetitive impact on your lower back is essential
- Movement techniques – bend, lift, carry, posture
– Bend your knees and hips, not your back
– Lift heavy objects using the correct lifting technique
– Carry larger loads in a comfortable rucksack using both shoulder straps, and avoid sling bags
– Posture – maintain a good posture – and avoid slumping in your chair, hunching over a desk, or walking with your shoulders hunched. If you work at a computer for long periods, ensure your chair and screen height are optimised - Breaks – take a short break from sitting every 30 minutes
- Stop smoking – it is thought smoking reduces the blood supply to the discs between the vertebrae, and this may lead to these discs degenerating (causing prolapsed or ‘slipped’ discs .. see below)
- Bed – check that your bed provides the correct support and comfort for your weight and build, not just firmness. An ‘orthopaedic’ (or lordotic) pillow may help to maintain a healthy overall spinal alignment
- Learn relaxation techniques – such as this breathing exercises to help manage stress. Stress is a major cause of back pain. Acupuncture may help.
4. When and how should I see a doctor or physio about back pain?
If it continues, many GPs have someone called a NHS musculoskeletal (MSK) ‘first contact physio’ (therapist) you can see, without seeing your GP at all. See if there is one at your local surgery. Many MSK physiotherapists operate a self-referral pathway online, or by telephone – i.e. you do not have to see the GP first.
They will be able to assess your symptoms, examine you, and recommend some useful exercises to help to alleviate pain – and organise an MRI if needed. They will also be able to arrange any necessary investigations and onward referral to a specialist (a spinal surgeon) if necessary.
5. How long should I wait for, before I see a doctor or physiotherapist?
If you have new back pain (and it is not too severe), unless you have one of the red flag symptoms below, it is often best to wait two weeks before seeking help, as it often corrects itself.
6. Back pain red flag symptoms
But .. remember sometimes back pain is a sign of a more serious problem. Here are some ‘red flag’ symptoms that are a concern. If you have these as well, it is important to see a doctor soon.
- Age <18 years and >60 years
- Bladder, bowel (inability to control your wee-ing or poo-ing) or sexual dysfunction
- Weakness or loss of sensation in the legs or arms
- Fever or weight loss
- Pain at night
- Trauma, or recent back surgery or epidural
- Other diseases – e.g. cancer, TB or HIV
- Drugs – including, anticoagulants, immunosuppression (drugs that suppress the immune system) and IV recreational drugs
- Severe new pain lasting over two weeks.
What are causes of back pain I should look out for? Here are two important ones.
7. What is a prolapsed (‘slipped’) disc?
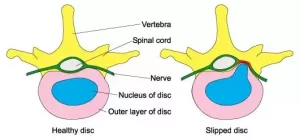
A ‘slipped disc’ occurs when the gel-like centre of one of the cushions between the vertebrae (building locks of spine) escapes from its outer casing. A fragment may cause pressure on one or more of the nerves which supplies the legs causing leg pain (‘sciatica’). As with most low back problems, the vast majority will rectify themselves with time.
 Prolapsed disc
Prolapsed disc

Spinal MRI: Prolapsed disc touching spinal nerves (not everyone needs an MRI)
In fact, 90% are better by six weeks. Those cases of sciatica which do not resolve with time and exercises, may benefit from an ‘epidural’ injection of anaesthetic and steroid medication. This can be a useful test both to confirm the cause of pain, and to provide long enough symptomatic relief for the problem to rectify itself.
Surgery to decompress the nerves may be offered when conservative treatment (rest, injections etc) has failed. Normally this can be done through a small cut in the lower back but it does carry some risk. Rarely, metal implants may be recommended if there is an underlying instability of the spine.
8. What is Cauda Equina Syndrome?
In extreme circumstances, compression of the nerve roots in the lower back which supply the legs, bowel and bladder can result in a condition called ‘cauda equina syndrome’. Urgent surgery is usually indicated. So if you have a rapid onset of severe back pain (especially if it spreads into both legs) associated with leg weakness and/or bowel, bladder or sexual dysfunction, you should go to your local A+E Department. Do not wait for appointment with your GP or anyone else.
After that, you need an MRI and to see a senior orthopaedic or neurosurgical doctor (consultant or registrar) ASAP, to plan an operation that may need to be done soon.
9. Do you need to have an MRI or see a surgeon?
A large majority of people with back pain do not need an MRI, or to see a spinal surgeon (e.g. neurosurgeon or orthopaedic surgeon).
10. Are back x-rays useful?
Rarely. The best test to diagnose a more serious problem is a spinal MRI. If you have any of the red flag symptoms above, you may need one soon. If you do not, your physiotherapist will normally arrange an MRI scan if your symptoms are persistent and do not respond to standard non-surgical treatment. Simple x-rays may be of additional use in selected cases.
Summary
We have described 10 facts about back pain. We hope it has been helpful. There is a lot you and the NHS can do.
Other resource
Back Care UK is a national back pain charity.

