How to write a good discharge summary (7 top tips)
Key points
- Think about why you are doing it, and who is the reader
- Describe the salient points of the admission, and in a logical structured way
- Paragraphed properly (3-4 sentences per paragraph)
- Do not include so much information that people will not read it. Less is more
- Relevant negatives (unless very relevant) and abbreviations are not helpful.
What is a discharge summary and what are they for?
It is the only piece of information the GP receives about your patients’ entire admission (anything from 1 day to many months). They need to have an understanding of key events and decisions that occurred.
First of all, be clear on why you are writing the letter. There are 4 reasons for the summary (all related to the ‘3 C’s: communication, communication and communication’):
- Communication with GP (or other health professionals) – to encourage action they need to take
- Communication with patient – to encourage action they need to take. Copy directly to the patient whenever possible
- Communication with hospital colleagues – in other departments, or if the patient comes in as an emergency
- Medicolegal record – i.e. a record of the admission.
Who writes them?
Writing discharge summaries is traditionally the task of junior (resident) doctors. They may have had formal or informal training about how to do them. Discharge summaries are often seen as a low priority for pressurised junior staff; who might not have had sufficient feedback and supervision in how to produce high quality summaries. So, you can do better.
Oh yes. GP’s are too busy to read War and Peace, and you are too busy to write it. Finding the balance will come with time and experience, but do NOT copy the entire text for every scan or put every blood test result.
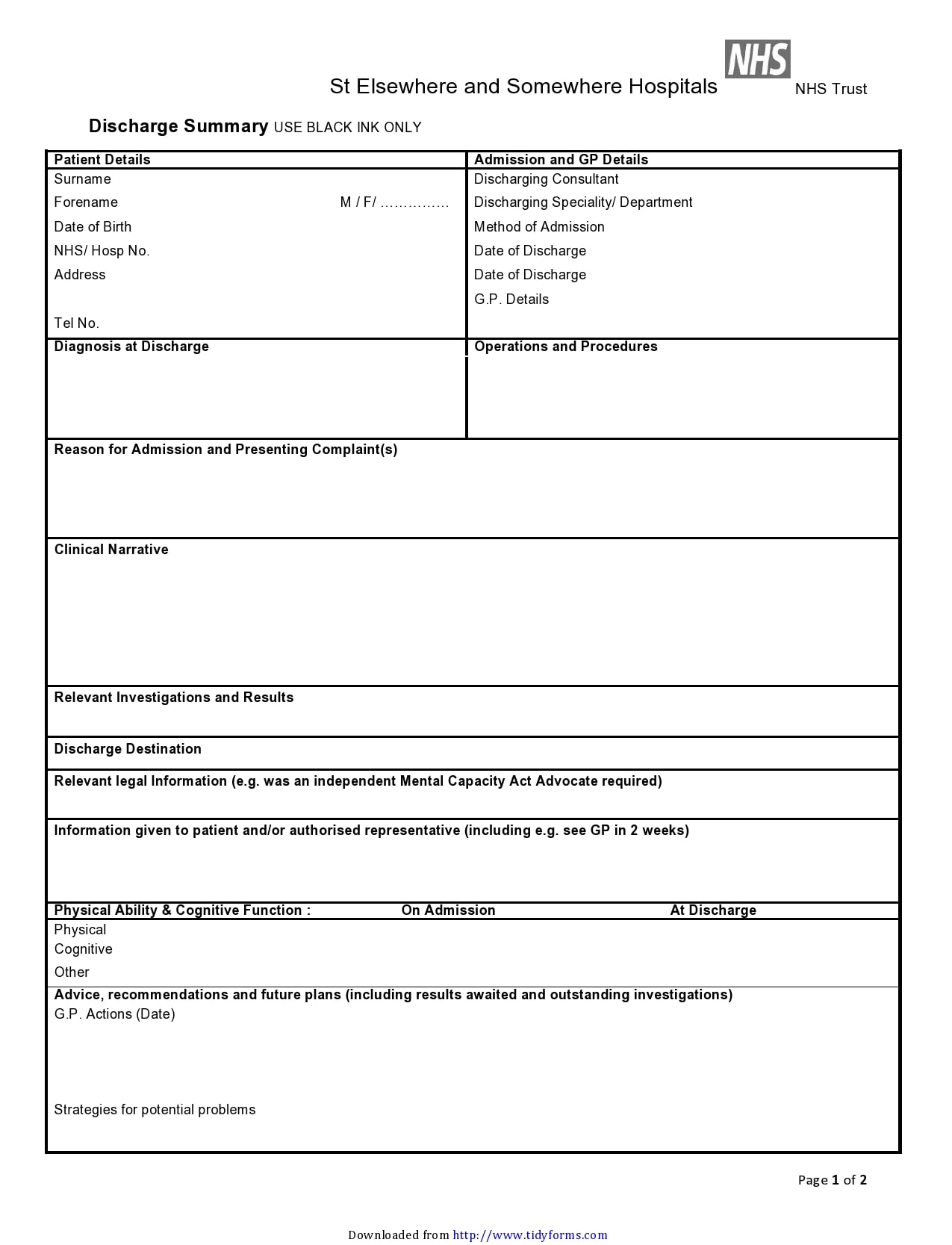
Now, let’s start. A good discharge summary should have 6 components:
Start – consultants name at the top (they take ultimate medicolegal responsibility for the patient’s care).
1. Patient details
- Which ward (and department)
- When admitted
- When discharged (or transferred).
2. Diagnoses
- Current diagnosis. Use precise diagnoses – ask your Consultant or Registrar if in doubt. Avoid jargon like ‘urosepsis’
- (Relevant) positive investigations
- (Relevant) past medical and surgical history
3. Management (procedures, operations, treatments, referrals)
- E.g. fluids and IV antibiotics
- Invasive investigations (e.g. biopsy or angiogram)
- Operations
- Complications (of disease or iatrogenic)
- Specialist referrals
- Community services arranged e.g. Home Help, District Nurse etc.
4. Discharge drug list
- Noting drugs stopped or started
- Old/new allergies.
5. Follow-up plan
- Make it clear what tests or results are outstanding – please do not ask the GP to chase them up
- If outpatient follow-up is being arranged with your team (or other teams). When and where
- Post discharge procedure or operation plan (if necessary).
Note. Again, please do not ask GPs to organise follow-up with your team or others. That is your job.
6. Action for GP or patient
- Action for GP – e.g. follow up blood tests – when (and action required if high or low)
- Action for patient (or family) – e.g. get resupply of new tablets.
Note. Again, please do not ask GPs to organise complex investigations (e.g. an MRI) or list for operations etc. Again, that is your job.
7. End – writers details
- Name (and bleep number)
- Rank
- Consultant you work for
- How to contact them (or consultant) if needed.
Example
This is an example of quite a good one.
Summary
We have described how to write a good discharge summary (7 top tips). We hope it has helped you. One final point to remember is that perhaps some time in the future, you will be on the receiving end and will appreciate a job well done.

