Hyperlipidaemia – 10 revision facts
Key Points
- Hyperlipidaemia refers to elevated levels of lipids in the blood, primarily cholesterol and triglycerides
- It is a major risk factor for atherosclerosis, which can lead to ischaemic heart disease (IHD) and stroke
- Management involves lifestyle modifications and pharmacological treatment, primarily with HMG CoA reductase inhibitors (statins)
- Early identification and treatment are crucial to reducing the risk of cardiovascular events.
 Cholesterol
Cholesterol
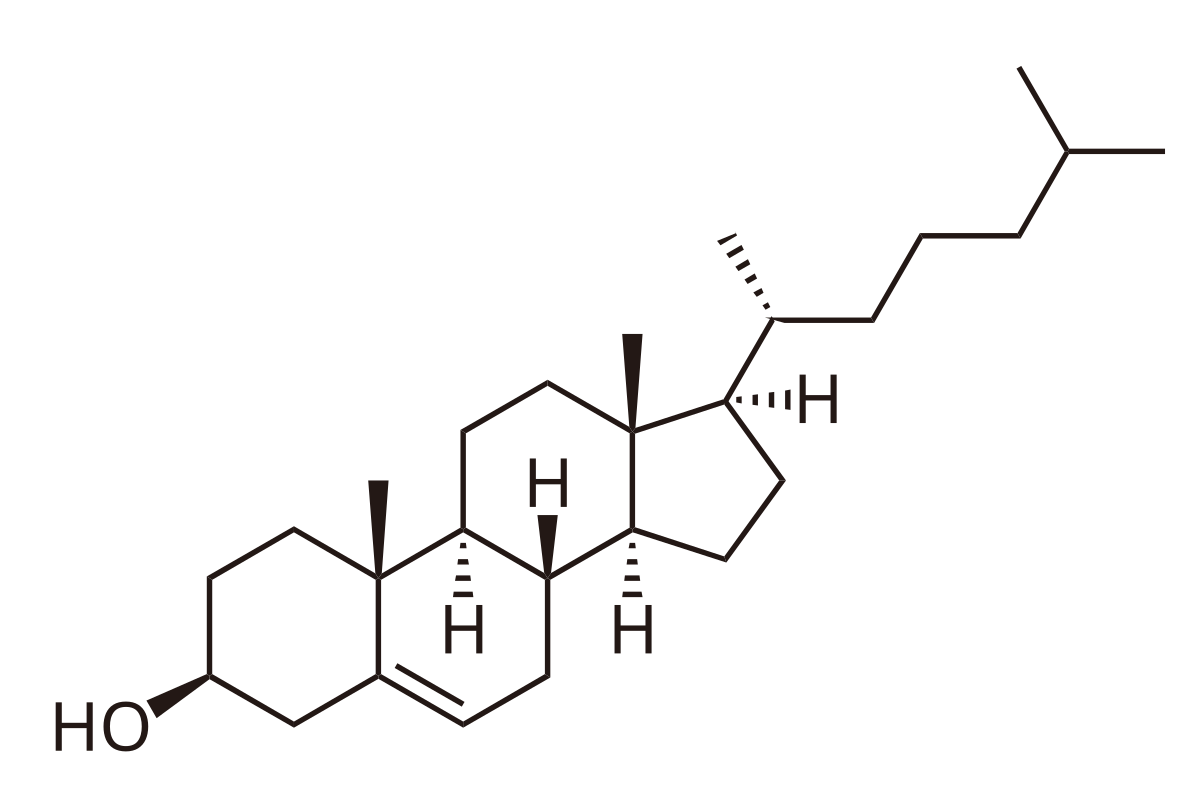
What is cholesterol?
It is a fat which all humans need to keep healthy. Many different cells make cholesterol. The liver makes about a quarter of the total. Its function is to help the body make cell membranes, many hormones, and vitamin D. It is not a disease. The diagram above is what it looks like as a chemical.
1. Definition
Hyperlipidaemia is the abnormal elevation of lipids in the blood, including cholesterol, triglycerides, or both. It can be classified based on the lipid profile:
- Hypercholesterolaemia: Elevated total cholesterol or low-density lipoprotein (LDL) cholesterol
- Hypertriglyceridaemia: Elevated triglycerides
- Mixed (combined) hyperlipidaemia: Elevation of both cholesterol and triglycerides.
2. Epidemiology
- Hyperlipidaemia is very common, affecting around 60% of adults, with variations based on age, sex, and ethnicity
- Men are more likely to have high cholesterol levels compared to women until menopause, after which the risk in women increases
- Age-related increase: Lipid levels generally rise with age, increasing the risk of cardiovascular disease
- It is a significant contributor to the burden of cardiovascular diseases, which remain one of the leading causes of death in the UK.
3. Risk factors
- Non-modifiable
- Age: Risk increases with advancing age
- Gender: Men are at higher risk earlier in life; risk in women increases after menopause
- Family history: Genetic predisposition plays a significant role, particularly in conditions like familial hypercholesterolaemia.
- Modifiable
- Diet: High intake of saturated fats, trans fats, and cholesterol
- Obesity: Particularly central obesity
- Sedentary lifestyle
- Excessive alcohol consumption: Contributes mainly to hypertriglyceridaemia
- Smoking: Lowers HDL (‘good’) cholesterol and increases total cholesterol
- Comorbidities: Diabetes, hypertension, chronic kidney disease (CKD), and hypothyroidism.
4. Causes
- Primary (genetic):
- Familial hypercholesterolaemia (FH): An autosomal dominant disorder characterised by high LDL cholesterol
- Polygenic hypercholesterolaemia: A common genetic condition resulting from multiple gene variations
- Familial combined hyperlipidaemia: Elevated cholesterol and triglycerides due to genetic factors.
- Secondary (acquired):
- Dietary factors: High intake of saturated fats and sugar
- Medications: E.g. corticosteroids, antiretrovirals, beta-blockers, thiazides, and oral contraceptives
- Medical conditions: Hypothyroidism, nephrotic syndrome, chronic kidney disease, liver disease, and type 2 diabetes.
5. Symptoms
- Asymptomatic: Most individuals with hyperlipidaemia are asymptomatic and are diagnosed through routine blood tests.
- Physical signs (in severe cases)
- Xanthomas: Yellowish deposits of lipid under the skin, particularly around the eyes (xanthelasma), tendons (tendon xanthomas), or over joints
- Corneal arcus: A grey-white ring around the cornea, often seen in younger patients with familial hypercholesterolaemia
- Hepatosplenomegaly: Can occur in severe hypertriglyceridaemia.

Corneal arcus

Corneal arcus and xanthelesma
Tendon xanthoma
6. Diagnosis
- History and physical examination: Assess for risk factors, family history, and signs of lipid deposits
- Risk assessment: Use scoring systems like QRISK3 to determine the risk of cardiovascular disease and guide treatment decisions.
Investigation
- Lipid profile: A fasting (and non-fasting) lipid profile measures total cholesterol, LDL cholesterol, high-density lipoprotein (HDL) cholesterol, and triglycerides
- Liver function tests (LFTs): Done before starting statin therapy to check baseline liver function
- U+Es: To assess renal function, especially if secondary causes like CKD/nephrotic syndrome are suspected
- Thyroid function tests: To rule out hypothyroidism as a cause of secondary hyperlipidaemia
- HbA1c and fasting glucose: To screen for diabetes, which can contribute to dyslipidaemia
- Genetic testing: Consider in cases of suspected familial hypercholesterolaemia, particularly in young patients with high cholesterol and a strong family history of early IHD or stroke.
Differential diagnosis
- Secondary hyperlipidaemia due to hypothyroidism, nephrotic syndrome, or diabetes.
- Primary genetic disorders like familial hypercholesterolaemia, familial combined hyperlipidaemia, or dysbetalipoproteinaemia.
- Drug-induced hyperlipidaemia: Caused by medications such as corticosteroids, antiretrovirals, or diuretics.
Desirable lipid levels
- Total cholesterol (TChol): 5.0 mmol/L or less. However, about 2 in 3 adults in the UK have a TChol level of 5.0 mmol/L or above
- LDL-cholesterol (‘bad cholesterol’): 3.0 mmol/L or less
- HDL-cholesterol (‘good cholesterol’): 1.2 mmol/L or more
- TChol/HDL ratio: 4.5 or less. That is, TChol divided by HDL-cholesterol. This reflects the fact that for any given TChol level, the more HDL, the better.
- Triglyceride (TG): 1.7 mmol/L or less (borderline high = 1.8 to 2.2 mmol/L).
As a rule, the higher the LDL-cholesterol level, the greater the risk to health. A blood test only measuring total cholesterol may be misleading. A high total cholesterol may be caused by a high HDL-cholesterol level and is therefore healthy. Thus it is important to know the separate LDL and HDL-cholesterol levels.
7. Treatment
- Lifestyle modifications:
- Diet: Encourage a balanced diet low in saturated fats and rich in fruits, vegetables, whole grains, and omega-3 fatty acids
- Weight management: Aim for a healthy BMI through diet and regular exercise
- Physical activity: At least 150 minutes of moderate aerobic activity per week
- Reduce alcohol intake: Particularly in patients with hypertriglyceridaemia
- Smoking cessation: To improve overall cardiovascular health.
- Pharmacological therapy:
- Statins: First-line treatment for lowering LDL cholesterol. E.g. atorvastatin, simvastatin, rosuvastatin
- Ezetimibe: Can be added to statins if LDL targets are not achieved or if statins are not tolerated
- PCSK9 inhibitors: E.g. alirocumab, evolocumab, for patients with familial hypercholesterolaemia or those who cannot reach LDL goals with other treatments
- Fibrates: Primarily used for hypertriglyceridaemia
- Omega-3 fatty acids: Useful for lowering triglycerides.
- Monitoring: Regular follow-up with lipid panels to assess treatment efficacy and compliance. Monitor for side effects of medications, particularly muscle symptoms with statins.
8. Complications
- Cardiovascular disease: Including IHD and stroke
- Pancreatitis: Associated with severe hypertriglyceridaemia (>10 mmol/L)
- Peripheral vascular disease (PVD): Can lead to claudication and other complications.
9. Prognosis
- The prognosis depends on the effective control of lipid levels and the management of cardiovascular risk factors
- With appropriate treatment, the risk of cardiovascular events can be significantly reduced
- Patients with familial hypercholesterolaemia have a higher risk of premature cardiovascular disease, but early identification and aggressive management can improve outcomes.
10. Prevention
- Healthy lifestyle: Maintaining a balanced diet, regular physical activity, and a healthy weight are key to preventing hyperlipidaemia
- Regular screening: Particularly in individuals with a family history of hyperlipidaemia or cardiovascular disease. QRISK assessments can guide when to start treatment
- Patient education: Encourage adherence to a heart-healthy lifestyle and compliance with prescribed medications.

