10 IHD (ischaemic heart disease) facts
In this article, we will provide 10 medical revision notes about ischaemic heart disease (IHD).
Key Points
- Ischaemic heart disease (IHD), also known as Coronary Artery Disease (CAD), is a leading cause of morbidity and mortality worldwide, characterised by reduced blood supply to the heart muscle.
- It is primarily caused by atherosclerosis of the coronary arteries.
- Risk factors include age, hypertension, smoking, diabetes, and hyperlipidaemia.
- Management involves lifestyle modifications, pharmacotherapy, and interventional procedures such as percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG).
- Prevention focuses on risk factor control, particularly through lifestyle changes and pharmacological measures.
1. Definition
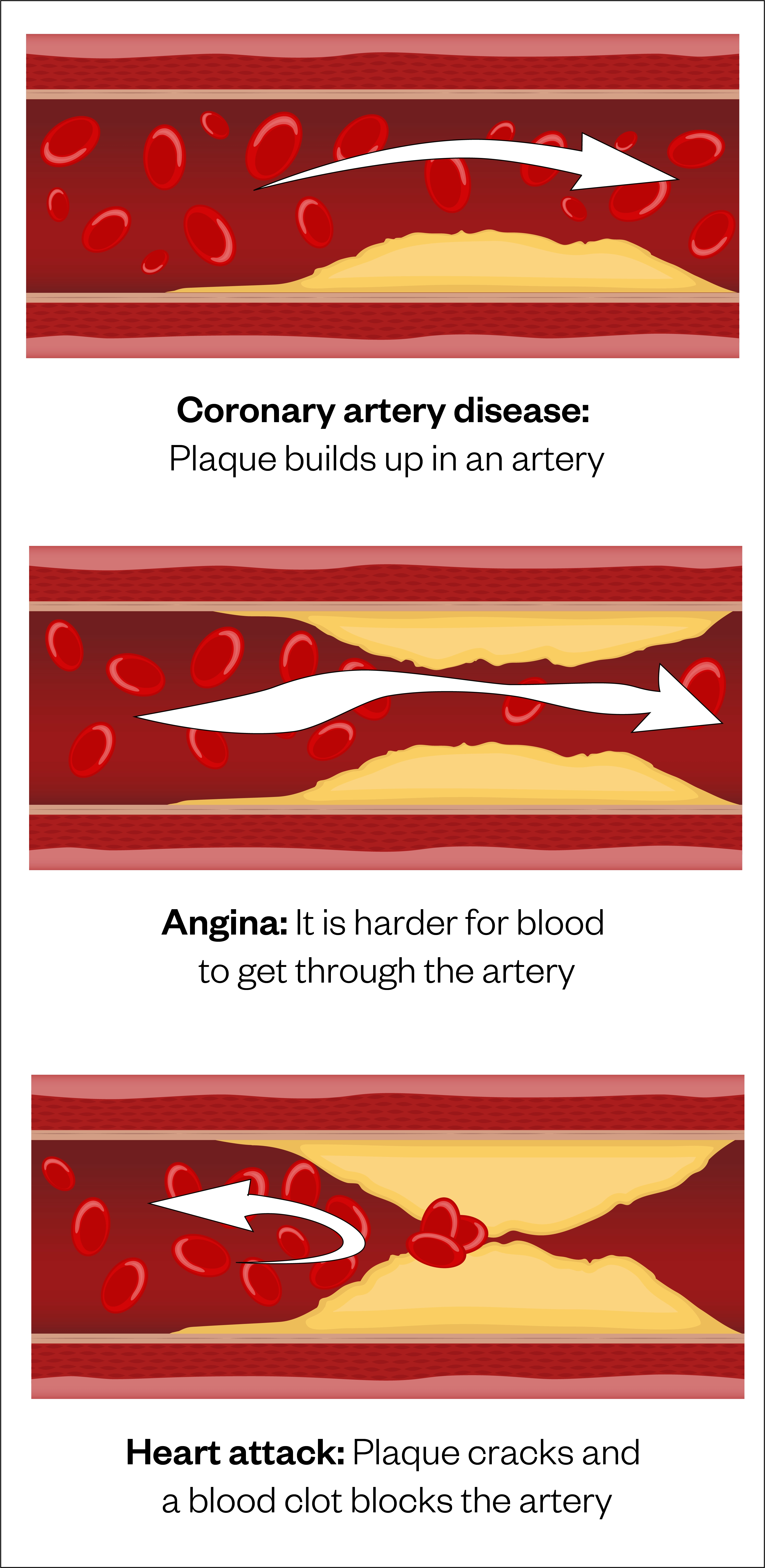
- Ischaemic heart disease (IHD), also known as coronary artery disease (CAD), occurs when the blood flow to the heart muscle is reduced because of a partial or complete blockage of the arteries supplying it with blood.
- This leads to myocardial ischaemia, which can manifest as angina, myocardial infarction (MI), or chronic heart failure (CHF).

Coronary arteries
2. Epidemiology
- Prevalence: IHD remains a major cause of morbidity and mortality globally, accounting for approximately 16% of deaths worldwide. In the UK, IHD is a leading cause of death, particularly among the elderly
- Age: The risk of IHD increases significantly with age. It is uncommon in individuals under 40 but prevalent in those over 65
- Gender: Men are more likely to develop IHD at an earlier age than women. However, the risk in women increases post-menopause
- Geography: Higher prevalence in developed nations, though rates are rising in developing countries posssibly due to lifestyle changes.
3. Risk factors
Non-modifiable
- Age: Risk increases with age
- Gender: Higher risk in men, though it evens out after women reach menopause
- Family history: A positive family history of premature IHD (in male relatives <55 years, or female relatives <65 years) increases risk.
Modifiable
- Hypertension
- Smoking
- Diabetes mellitus
- Hyperlipidaemia
- Obesity/physical inactivity
- Poor diet: Diets high in saturated fats, trans fats, and cholesterol
- Excessive alcohol consumption.
3. Causes
- The primary cause of IHD is atherosclerosis, a process where lipid-laden plaques build up within the coronary arteries, leading to narrowing (stenosis) and reduced blood flow
- This can result in myocardial ischaemia, particularly during periods of increased demand, such as exercise or stress
- Other less common causes include:
- Coronary artery spasm (Prinzmetal’s angina)
- Coronary artery dissection
- Embolism or thrombosis in the coronary arteries.
4. Symptoms
The presentation of IHD can range from asymptomatic to acute coronary syndromes (ACS). Common symptoms include:
- Angina:
- Chest pain or discomfort, often described as pressure, tightness, or squeezing; classically radiating down the left arm (or into neck or back)
- Typically precipitated by physical exertion, emotional stress, or cold exposure
- Relieved by rest or nitrates.
- Shortness of breath: Especially on exertion (sign of heart failure)
- Fatigue: Generalised tiredness or weakness
- Palpitations: Awareness of heartbeat (in atrial fibrillation or other arrhythmias)
- Acute presentation (Acute Coronary Syndrome, ACS):
- Unstable angina (myocardial ischaemia): Angina at rest, prolonged, or worsening
- Myocardial infarction: Severe, prolonged chest pain not relieved by rest or nitrates; accompanied by symptoms such as sweating, nausea, or vomiting (these symptoms help distinguish infarction from ischaemia).
5. Diagnosis
The diagnosis of IHD is based on a combination of history, examination and diagnostic investigations. Important aspects include:
- Detailed history of symptoms, including nature, duration, and triggers of chest pain
- Assessment of risk factors and family history
- Physical examination may reveal signs of hypertension, hyperlipidaemia (e.g. xanthelasma), or other related conditions.
Investigation
- Electrocardiogram (ECG): Look for signs of myocardial ischaemia (e.g. ST-segment depression, T-wave inversion) or infarction (e.g. ST-segment elevation, pathological Q waves).
- Blood tests:
- Cardiac biomarkers: Troponin levels detect myocardial damage
- Lipid profile
- Blood glucose/HbA1c
- Exercise stress testing: To assess for exercise-induced ischaemia
- Echocardiography: Evaluates cardiac function, detects wall motion abnormalities
- Coronary Angiography: Gold standard for diagnosing coronary artery stenosis
- Cardiac CT or MRI: Non-invasive imaging options to assess coronary anatomy and myocardial perfusion.
Differential diagnosis
- Gastroesophageal reflux disease (GORD)
- Musculoskeletal pain: Costochondritis
- Pulmonary embolism
- Pericarditis
- Aortic dissection
- Panic attacks or anxiety disorders.
7. Treatment
Treatment of IHD involves a combination of lifestyle changes, pharmacological therapy, and interventional procedures:
- Lifestyle modification
- Smoking cessation, healthy diet, regular exercise, weight management, and stress reduction.
- Pharmacological therapy
- Antiplatelets: Aspirin, clopidogrel
- Statins
- Beta-blockers: To reduce heart rate and myocardial oxygen demand
- ACE inhibitors/ARBs: For hypertension and chronic heart failure
- Nitrates: For angina relief
- Calcium channel blockers: Alternative to beta-blockers.
- Interventional procedures
- Percutaneous coronary intervention (PCI): Angioplasty with stent placement to restore blood flow
- Coronary artery bypass grafting (CABG): Surgical revascularisation for severe multivessel disease or left main coronary artery stenosis.
8. Complications
- Acute myocardial infarction (MI)
- Heart failure (acute and chronic)
- Cardiac arrhythmias: Atrial fibrillation, ventricular tachycardia/fibrillation
- Sudden cardiac death
- Chronic angina: Reduced quality of life.
9. Prognosis
- The prognosis of IHD varies based on disease severity, comorbid conditions and treatment adherence
- Early diagnosis and effective management can improve outcomes and reduce the risk of complications
- Patients with stable angina have a better prognosis compared to those who experience a myocardial infarction or develop heart failure.
10. Prevention
Primary prevention
- Addressing modifiable risk factors, such as smoking cessation, healthy eating, regular physical activity, and maintaining a healthy weight
- Regular screening for hypertension, diabetes, and dyslipidaemia, especially in high-risk groups
- Prophylactic use of statins and antiplatelets in high-risk patients.
Secondary prevention
- Strict control of risk factors in patients with known IHD to prevent recurrent events
- Adherence to prescribed medications
- Cardiac rehabilitation programs to improve exercise tolerance and quality of life.
Summary
We have provided 10 medical revision notes about ischaemic heart disease (IHD). We hope it has been helpful.
Top Tip
Coronary angiography is not indicated as a primary prevention tool, i.e. there is no benefit in ‘looking for’ IHD in asymptomatic patients.
Other resource
MyHSN ischaemic heart disease podcast (2024) – 9 min, 47 sec

