Jammed NHS hospitals – five problems and solutions
In the UK, there were 7.46 million people waiting for an operation (procedure or treatment) in December 2024. This is over 10% of the population.
Also, the corridors in our A&E departments are full of the frail elderly on trolleys waiting for a bed. Ambulances cannot pick up the next potentially seriously ill patient.
How bad is it in A&E?
Pretty bad. In fact, after a decision to admit, 20,000 people a month spend over 12 hours on a trolley in a corridor. These are hard trolleys in an A&E corridor, quite unsuited to the frail elderly who rapidly develop bed sores. Almost all patients that pass through ‘Majors’ in A&E fail the 4 hour target now.
When A&E is full, and the corridors are full, we sit sick people in chairs. Ambulances cannot release and handover their patients. There is no where for them to go. When the hospital is blocked, surgery and cancer care does not happen properly.
These are things we hear and read about daily in our media. It is all true. But why do we have these problems and what can be done to fix them? MyHSN believes there are five major things that need to be sorted. Sorting one of them will not help, as these five are linked (i.e. affect each other).
They are written in order of importance, with 1, 2 and 3 being of primary importance. But until we address all 5 (especially 1, 2 and 3) there will be no significant unjamming of our hospitals .. and no ability to clear the surgery and cancer waiting lists, to a level appropriate for a developed countries. Other countries ‘like us’ do it. Its possible.
Interestingly, only one (the first one we discuss) will cost a significant amount of money. The rest are to with administration of the NHS. They are organisational issues that need ‘cultural change’ – i.e. of traditional work practices – to sort.
Let’s examine why this is so, and what can be done. First of all let’s look at ourselves, the docs.
Doctors blame the system but do not look at themselves
Doctors are very good at blaming the government, DHSC and NHS England. They rarely look at themselves. They want more money, staff and beds. But, the big BUT is nearly 50% or more possible planned activity is wasted every week, because of doctors’ traditional work practices.
That is a choice. The choice of them, and the BMA and Royal Colleges. Doctors choose to work in a way that suits them, not the public. Just as they choose how many patients they see, they choose to work a 5 day week. Hospitals don’t make them work in this way. Google, Premier Inn, Booking.com, Tesco and Amazon are able to work in modern ways, by using rotas. As do the police, ambulance service, fire brigade and armed services. So can we.
Ok, let’s go back to why NHS hospitals are jammed, and go through the big five problems and solutions, one by one.
1. Emergency and elective care
They need to be separated. Full stop.
Without separating these, we cannot deal with the NHS waiting lists. Full stop. At the moment we mix ‘hot’ and ‘cold’ care, e.g. medical and surgical emergencies (like someone with pneumonia or appendicitis) with elective surgery (such as a hip replacement). We always prioritise the frail and most vulnerable as they are more likely to die. These emergencies come in and mean that elective surgery is cancelled.
In a normal large hospital, there will be about 30 (say 20 surgical and 10 orthopaedic emergency) operations a day. But they will also be 50 planned operations, with a heavy orthopaedic component (hip replacements etc). And many of these get cancelled, especially on Mondays (see below).
Solution – split elective and emergency care
Through COVID-19, we learnt that private hospitals could carry out NHS elective surgery near acute hospitals. We could do this again, so that you have elective surgery carried out in a different building. Private operators are good at running such ‘surgical treatment centres’ (or ‘hubs’). The proposed public and private sector hubs would never compromise their beds for emergencies.
In the future, we should build two different NHS buildings side-by-side; one an acute hospital, the other a surgical treatment centre. In the meantime, private hospitals in the UK (and abroad) could provide significant beds. And, we could start separating buildings in current acute hospital sites. Many trusts have several sites and could move services to their other sites. This will involve building work.
The new subregional Integrated Care Boards (ICBs), are (sort of) merging hospitals. They could encourage the division of hospitals to happen. But the ICBs do not have the power to do so at present. We could accelerate that power, but that will require another Act of Parliament.
In the future, the only operations happening at acute hospitals should be emergency ones, and high risk elective ones (where an ICU bed is predicted to be required post-operatively).
2. Seven-day working week (and time of day problem)
Hospitals in the UK will never (ever) function properly – in terms of either elective or emergency care – without a 7 day service. Repeat .. never (ever) function. No target will be achieved. Financial balance will not be achieved. Both are mathematically impossible now, with how we run the NHS at present. Much of that is a choice, and its within our gift to choose another path.
For example, hospitals do not have the full complement of staff at weekends and bank holidays. They should. As should general practice, mental health, dentistry, the lot. This is 2025. MyHSN thinks we (all NHS staff) should provide a full 7DS, with working days being identical.
Why? People get ill 7 days a week. Disease does not recognise weekends and bank holidays. Much of the rest of society works the same 7 days a week now. It’s easier to buy some asparagus at weekends than see a doctor. We would not tolerate a police force, fire brigade or army that had weekends off.
The most senior hospital doctors (consultants, and their deputies called registrars) are present in small numbers at weekends and on bank holidays. A previous study showed that there were 86 consultants on site in a hospital on a Wednesday (on average), with 12 at weekends. One hospital had 63 on a Wednesday and none at the weekend. They should be there in normal numbers, leading full teams. Also getting key investigations like scans is harder.
This overlaps with point one. Emergencies (medical and surgical) continue to be admitted at weekends, but we only discharge 60% of normal on a Saturday, and 40% on a Sunday.
Therefore, because of the lack of a split between emergency and elective care, and the lack of a seven-day working, these patients clog up beds in the surgical wards – and planned elective operations (including cancer ones) on Monday are cancelled.
Mondays are chaos in most hospitals. In fact hospitals don’t even work a 5 day week, it’s about 3.5. Saturday/Sunday = not much. Monday = chaos, sort out weekend admissions. Tues-Thurs, they work reasonably well. Friday, half day, job done. It is like a repeating Kafka-esque nightmare. Groundhog Day NHS style.
It is not just hospitals. GP surgeries are 5 day services; open Monday – Friday 8am-6.30pm excluding bank holidays. There is 24 hour GP cover but this is not by your local surgery. This also means GPs come into chaos on Mondays. Also, dentists are open even less hours than GPs.
Access to patients’ GPs is not great at present. And when you cannot see your GP in good time, inevitably you may go to your local A&E. That is understandable. That again is fixable, partly by a 7DS.
Back to hospitals. Furthermore, operating theatres are poorly used on Friday afternoons and at weekends, which is a waste of a valuable resource. Surgeons do not do planned complex operations on Fridays, preferring to make that a ‘management/audit’ day. This is because they know their patients will not be reviewed routinely on Saturdays and Sundays.
All of this is also a huge waste of a public resource.
Being ill at weekends is also dangerous. You have an 11% increase in mortality if you are admitted at weekends. This is the evidence.
The most dangerous period is the long Easter weekend, when the NHS largely stops for 4 days. This is followed by the Xmas/NY period, which is almost as dangerous. Interestingly the weekend effect exists for all illnesses: medical or surgical, elective or emergency, low or high risk – in all countries. Mortality starts to go up on a Friday, peaks on Saturdays and Sundays, and is up a bit on Mondays, as we sort ourselves out.
Time of day problem
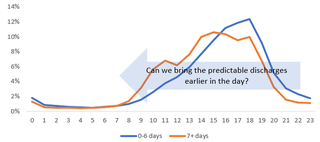
The peak of discharge time is 5-6pm (see graph below), with significant numbers going home 7-9pm, getting home very late at night. This relates to traditional work practices, e.g. a. the order in which patients are seen, and b. clunky and slow IT which makes it hard for the junior (resident) doctors to do the e-discharge summary at TTOs in good time.
So, for an example, a ward round goes like this ..
9am. Ward round starts and 30 patients seen in numeric order
10am. Senior doctor and discharges patient in bed 7. That patient may have been a ‘quickie’ (and if seen first could have left before lunch)
12pm. Ward round finishes
1pm. Junior docs (JDs) return after lunch, with many jobs to do
3pm. JDs start e-DS and TTOs. This is a unpopular and slow task (partly as they don’t know the patients, as they work strange shift patterns that do not lead to continuity)
5pm. JDs leave, with many tasks half-done
6pm+. patient discharged at 10am, may leave.
Solution – a 7 day NHS (identical every day)
The time has come for the NHS to grow up, reflect social change, modernise and reform. We need to move on from 20th Century medicine. Fact one. People get ill at weekends. Fact two. Google, Premier Inn, Booking.com, Tesco and Amazon work at weekends. Fact three. So should we. This includes hospitals, general practice, mental health, community and social care (see below) – elective and emergency – the whole shebang. The work-life balance of senior staff should not be our major priority. It is at present.
NHS England tried to start the journey towards a 7DS in hospitals in 2013-15. It failed, famously leading to a junior doctor strike. We need to have another go.
Many say ‘we need more doctors and nurses’. But the latest OECD analysis of healthcare in developed countries, does not support this case (well, maybe a few more doctors). We need to be cleverer how we use them, cleverer with rotas. Tesco does it. No one makes them. So can we.
How? There are many ways. A simple solution is to divide the NHS workforce in two: both work a four day week; one Mon-Thurs, the other Thurs-Sun. Change shift pattern every 4 months, first Monday in August, December and April – so no one works every Xmas etc. Simple.
We should pair up hospital consultants (within something called an ‘annualised contract’), so we do not lose their productivity when one is away. Most clinics, procedure or operating lists are cancelled when they are away (8 weeks a year). Because of that, the NHS loses nearly 20% of available activity a year. This also has a significant effect on waiting lists. Employing more doctors, nurses etc will not bring that back, unless traditional work practices change.
As we lose an additional 2/7 (30%) of available activity by not working properly at weekends, that’s a total of nearly 50% or more possible planned activity that is being wasted. This is highly inefficient. Would Tesco’s open 50% of the time?
It is not fair that only hospital doctors and GPs are in this ‘brave new 7 day NHS world’. It needs to be all staff. Repeat all staff. Nurses, AHPs, technical and admin staff, managers, community and social care .. the lot. And politicians.
Solution (time of day)
This needs a radical rethink. It may be possible to use A1 and computer-technology to: a. create e-DS with one click of the computer; and b. send TTO from hospital’s EPR directly into patients phone, GP and named pharmacy computer – so patient can pick up any new tablets in <48h of discharge.
There may need to be a different system for time-dependent drugs – e.g. insulin, anti-Parkinsons and epilepsy medication.
3. Social care
The NHS cannot be discussed without discussing the role of councils in social care as that has a huge effect on hospitals in particular. Why is that so?
The term ‘Department of Health and Social Care’ is a misnomer. Health does not run social care in the UK, and that is a huge problem. It is the Department for Levelling Up, Housing and Communities (i.e. local government, the councils). It has a different (smaller) budget, different processes, IT, email addresses, priorities, loyalties and traditions – different everything.
If it was the NHS, the 25% of patients in hospitals who are stuck there – labelled ‘medically fit for discharge’ and ‘waiting for social’ – would not be there. We call these ‘complex patients’ and they are just as (or more) important than the ‘simple patients’, where discharge is straightforward. Discharging the complex patients in good time would free up huge resources to deal with our over 7 million patients waiting for operations.
Who are these patients? They are people, us, our frail elderly. They are your parents and grandparents (and ours) – waiting for care arrangements to be in place, to allow their safe discharge from hospital. They need to go to a nursing home, or for carers to be arranged in the home. It is the councils role to provide that, not the NHS.
But, councils, as we all know, are strapped for cash. Also, crucially, unlike the NHS, their funding is not linked to population growth and they have to stay in budget every year. The NHS’s budget has the significant advantage of being linked to population growth; and crucially does not legally have to stay in financial balance. So most hospitals and ICBs that fund them are therefore effectively bankrupt every year and that is tolerated. Lack of financial rigour leads to sloppy accounting and inefficiency.
Even though the council organises social care and pays for some of it, the public have to contribute significantly to long term social care – if necessary by selling their houses. This is very unpopular. But on the other hand, unfortunately, most UK citizens are not willing for their frail elderly parents and grandparents home to live with them, especially if it will affect their lives, jobs and careers. They cannot have it both ways. In the end, someone will have to pay for it.
Another issue is that social care will not take patients back at weekends. This is ironic as the beds in nursing homes and carers are still there and available at weekends. But we cannot discharge these complex patients at weekends, further jamming hospitals and lengthening waiting lists. The other irony is that the reason they do not often take patients back is that they think (correctly) that the NHS does not work at weekends, so just copy us. We need all the social care managers to work at weekends to ‘OK’ theses discharges. They do not, copying our senior doctors and managers. They think ‘what is the point?’ if they don’t.
An example
The social care and health systems do not connect between councils and hospitals. For example, if you have a frail and elderly person in a nursing home who fractures their neck of femur and is sent to hospital, they take priority over a planned operation (competing for that bed).
Four weeks later when they are ready to go home, they are stuck in hospital at £400 a day. Why won’t nursing homes take them back? It is because everyone gets paid.
The hospital is paid £400 a day to keep them there and the nursing home is paid for the bed even if no one is in it. If everyone’s getting paid then there is no incentive to get people back.
Also, if they have been transferred to a larger more distant hospital for the operation, the original referring smaller local hospital – with links to its local (council-led) social care system – has no incentive to take them back, as a bridge to the original nursing home. And the current hospital has no links to the original council system. They are stuck.
Solution – move social care into NHS and run it 7 days a week
The budget for health is over £180 billion a year (10% of GDP, like most developed countries), versus about £30 billion for local government. This reflects our society’s priorities. The solution is to put social care into the NHS (and run it 7 days a week), and make hard choices regarding what we prioritise. We think the state (via the NHS) should pay for all social care, if necessary through a significant increase in general taxation, so people do not have to sell their homes.
4. Information technology
Successive governments over the past 20 years have tried to create a national NHS electronic patient record (EPR) and this has failed. On a local and sub-regional level, the data are not compatible.
Hence GPs, hospitals, pharmacies, mental health and ambulances do not know what each other is doing. The public are well aware of this issue and are fed up with our excuses; with hospital doctors saying “sorry, I cannot read your GP’s computer” and vice versa, etc. This leads to many mistakes, especially related to prescribing medicines.
Theoretically, it’s very simple to do when you have numbers in thousands and tens of thousands. However, when you have millions of patients with millions of pieces of information, it becomes much more difficult. These things are surmountable with money, and of course Google, Tesco and Amazon have done it. However, the NHS has substandard systems.
Another issue is that many patients get appropriate care and advice from their GP but then use A&E for a second opinion. By knowing what has gone on in primary care (with better IT), we could more easily deflect such patients away and hopefully teach some behavioural changes.
Solution – subregional (ICB-based) EPRs, eventually linked up nationally and to NHS App
Many hospitals in the UK are bringing in mainly American EPR systems now, including Cerner and EPIC. As they come online, we need to then link them up across the country. At the same time, we need to link the EPRs to the very good NHS App (now on the phones of over 30 million people, thanks to COVID-19).
The ICB system is ‘right size’ for the geographic limits of a a subregional EPR. Linking ICB’s geography to county councils will also help. ICBs should drive these IT changes through, even if hospitals are initially reluctant as they cannot see a short-to-medium term benefit.
How much will it cost? Apart from the initial purchase cost of over £200 million even for a cheaper system (for a large hospital group), it can cost £7 million a year to maintain it. Once you start scaling that up, the cost is not small, but not huge either = £8.4 billion for 42 ICBs in England and about £300 million a year to run them.
So, yes, they are expensive. But we need to accept that and buy them. Anyway, this cost is tiny compared to the amount of money we spent on COVID-19. We spent £13 billion on PPE alone. Thats a lot of plastic pinnies.
5. Regional substructures (and pathway integration)
Most NHS organisations have a regional substructure. Unfortunately, for historical reasons, they are different in number, and completely different geographically. Hence there are, in England: 13 Health Education England regions (called LETBs or ‘deaneries’), 10 Ambulance Trusts (14 in UK), 9 UK Health Security Agency (public health) regions, 7 NHS England regions, and 4 NHS Health and Justice (prisons etc) regions. It’s mad.
It is also very difficult to integrate pathways that cut across all these organisations.
COVID-19 exposed this lack of connection and co-operation. There were stories of senior staff in the same building, with responsibility for the same bit of the country, who did not know they were in the same building; but had been emailing intermittently for years. This may have contributed to the UK’s poor performance.
This relates to our over 400 years of stable democracy, which is both good and bad. It leads to geographical and operational chaos (that is hard to change). But at the same time, it is very fair as systems are so complex that no one is really in charge, with power spread out. No one really runs the NHS.
None of these regions are linked up and have little connection with the 300+ councils. These facts explain why the NHS feels, to both staff and the public, like a huge machine of 7+ massive silos that do not know each other, or talk to each other. They are right. They do not. They could.
These organisational boundaries currently create barriers for patients to move to the right care setting. So we need better and integrated care pathways facilitated by co-terminous and organisational streamlining. Let us look how it could be done.
Solution – single regional substructure built around 7 NHS regions, and merge ICBs with county (or equivalent) councils
It would be hard but it is possible to start again, and rebuild the system around the 7 NHS England regions. HEE, UK-HSA, NHS H&J (and most other arms-lengths bodies) and the ambulance trusts, should have the same regional structure.
Each region will have about 7 subregional ICBs, which could take over social care from the relevant council. We could even align the geographical boundary of an ICB to be the same as the associated county (or equivalent) council. It is possible.
Also, an approximately 1 million population subregional ICB is about ‘right size’ as it can align with counties which are similar. This has been tried before in the NHS in the 1974 major reorganisation (first one since 1948). This created a similar subregional entity called ‘Area’ that worked well with the counties (they were not daft) but was then abolished in 1982 (which was daft); when the then government wanted to cut red tape and reduce management costs. Interestingly, contrary to popular opinion, the NHS spends relatively little on ‘management’. It is about 3% of the budget, a lot less than most large organisations and industry.
The ICBs could also take the lead regarding bringing in points 1 and 2 (split of elective/emergency care and a 7DS). For example some sites in an ICB can be converted to elective care only. Also there is no point if one hospital (including A&E) works 7 days and the others (with A&Es) do not. The former will flow better, and ambulances within an ICB will detect that and take more patients there, defeating the point. It needs to be ‘all in’ to work. That includes general practice and social care.
Unfortunately the DHSC and NHS England do not seem to have made either splitting emergency and elective care, or a 7DS, as a priority for ICBs. Presumably they don’t want to ‘upset the doctors’ and challenge the traditional work practices described above. And the power for ICBs to do anything off their own back is limited.
NHS funding mechanism. It’s time to change it
In other words, the NHS could become ‘7 regional NHS services’, with less central control, i.e. NHS England would have to be disbanded. Other developed countries like Australia have done this. A social insurance based system like in the Netherlands and Israel where there are no significant waiting lists may be a better funding model. In such a system healthcare is still free for less well paid people.
The NHS’s funding system is largely the same as in 1948 and is no longer appropriate for our country. Neither of our main parties have been brave enough to look at alternative systems. It is no coincidence that both Australia and Israel have had a significantly better death rate from COVID-19 than us, because their health services are better organised than our NHS. It helps that they are both ‘young countries’ of course.
As a country, in all spheres, we have allowed ‘the centre’ (London-based government) to dominate current and long-term planning and funding – including the NHS. The NHS is famous for short term national fixes. They no longer work. The problems are too deep-seated and in the ‘too difficult’ box.
Four main deep drivers of health need (and expense) – and the future
These are the four main deep drivers: Population growth, Age, disease Complexity – especially chronic disease in the elderly, e.g. diabetes and dementia; leading to more medical advances (drugs/technology) – and public Expectation. At MyHSN we call this ‘PACE’.
But none of those things can be solved. So MyHSN prefers to look at solutions.
In summary we have explained why NHS hospitals are jammed, and gone through the five problems and solutions.
In short, the NHS needs to modernise, join the 21st Century, give the public the healthcare they deserve, and one that is appropriate for a developed country.
Come on docs, let’s lead – not follow and blame everyone else – and sort this out for the general public. Ask yourself, what are you, your department, your hospital, your region doing today, to solve these key NHS problems. Let’s stop blaming the government, NHSE etc, asking for more and more money and staff. Let’s all pull together and start sorting The Big Five. Yes we can.
The Big Solution
In the view of MyHSN, the time has come for the Big Solution, i.e. a radical conversion of the NHS to a social insurance system like in the Netherlands. Anything less, will have no (or little) effect. The alternative? Vast investment using either huge tax rises or moving that money from other vital government departments. This would not be popular.
Summary
We have described Jammed NHS hospitals – five problems and solutions. Let’s go Dutch! We hope it has been helpful.
Other resource
The NHS
A new NHS for a new age: let’s go Dutch
How to convert the NHS into a (Dutch-style) National Health and Social Service

