Why is shaking the patient’s hand a good diagnostic practice?
The hands provide readily accessible information that may not be available through other history/examination, and they offer clues to a patient’s physical and mental health.
A good introduction is vital in medicine. And you should begin all physical examinations by reaching for the patient’s right hand with both of yours. Why? Starting with a handshake is friendly, gains patient trust, and is part of the examination.
We will now go through diagnoses that can be made by the handshake, focussing on tremors, nails, fingers, hands and palm. Each section will be in alphabetical order rather than most common first etc.
How to do a medical diagnostic handshake
There are 4 stages. As well as giving a friendly greeting ..
- Look at general demeanour of the patient – are they SOB, have oedema, in pain? Why in a wheelchair? What are they reading? Why?
- Before the handshake – look for tremors – does it get better or worse on intention?
- Look and feel: nails, fingers, palm and hand
- Take the pulse.
- The handshake is not something done in isolation. Think about your posture and eye contact as you do it
- Are the hands moist and warm? – thyrotoxicosis? look for tremor, eye signs, goitre; phaeochromocytoma??
- Is the patient unable to let go your of hand? – think myotonia, not to be confused with the grasp reflex in frontal lobe disease. Look for other signs of myotonic dystrophy, e.g. hatchet face, cataracts, baldness, myopathic facies.
But. Before the handshake – look for tremors
It is very important to look for tremors. There are two broad groups:
Rest tremors (better on intention)
- Parkinson’s disease
- Parkinson’s plus syndromes (rest tremor is less common)
- Drug-induced parkinsonism (neuroleptics, metaclopromide, and phenothiazines)
- Long-standing essential tremor
- Wilson’s disease.
Action tremors (worse on intention)
- Cerebellar disease
- Metabolic disorders (thyrotoxicosis, phaeochromocytoma, hypoglycaemia)
- Drug-induced parkinsonism (lithium, amiodarone, β-adrenergic agonists)
- Toxins (alcohol withdrawal/excess, heavy metals)
- Neuropathic tremor (neuropathy).
Nails
Acral lentiginous melanoma (involving nail)
While acral lentinginous melenoma is often seen anywhere on the palms, soles, and even in the mouth. When it occurs within the nail, a clue that this is melanoma is involvement of the periungal regions as seen in this picture.
Transverse depressed ridges seen in severe infection, MI, hypotension/shock, hypocalcemia, post-surgical, malnutrition and with certain chemotherapy.
Clubbing
Clubbing of the nails is soft tissue swelling of the terminal phalanx, resulting in the straightening of the angle between the nail bed and the nail. The angle between nail plate and proximal nail fold is greater than 180 degrees.


Causes of clubbing include:
- Respiratory
- Lung cancer. Clubbing is in general an ominous sign for this, and remember ‘beware of the yellow clubbed digit’ (yellow from nicotine, and clubbed from cancer)
- Suppurative lung disease (bronchiectasis, cystic fibrosis, lung abscess and empyema)
- Pulmonary fibrosis (and its many causes)
- Asbestosis/pleural mesothelioma
- COPD IS NOT A CAUSE OF CLUBBING (if you seen clubbing in a COPD patient, think lung cancer).
- Cardiac
- Congenital cyanotic heart disease (L to R shunts)
- Infective endocarditis
- Atrial myxoma.
- Gastrointestinal
- Inflammatory bowel disease
- Primary biliary cirrhosis
- Coeliac disease (and other cause of chronic malabsorption)
- GI lymphoma.
- Other
- Thyrotoxicosis (thyroid acropachy)
- Hereditary.
Koilonychia (‘spoon’ nails)
This is a deformity of the nails where the central portion of the nail is depressed and the lateral aspects of the nail are elevated. It can be due to chronic iron deficiency anaemia, secondary to malnutrition, worms, coeliac disease, gastrointestinal blood loss, and malignancy.
Leukonychia
This is most commonly caused by minor injuries, such as nail biting, or may occur while the nail is growing. It also may be caused by calcium deficiency, and hypoalbuminaemia of chronic liver disease (see below).
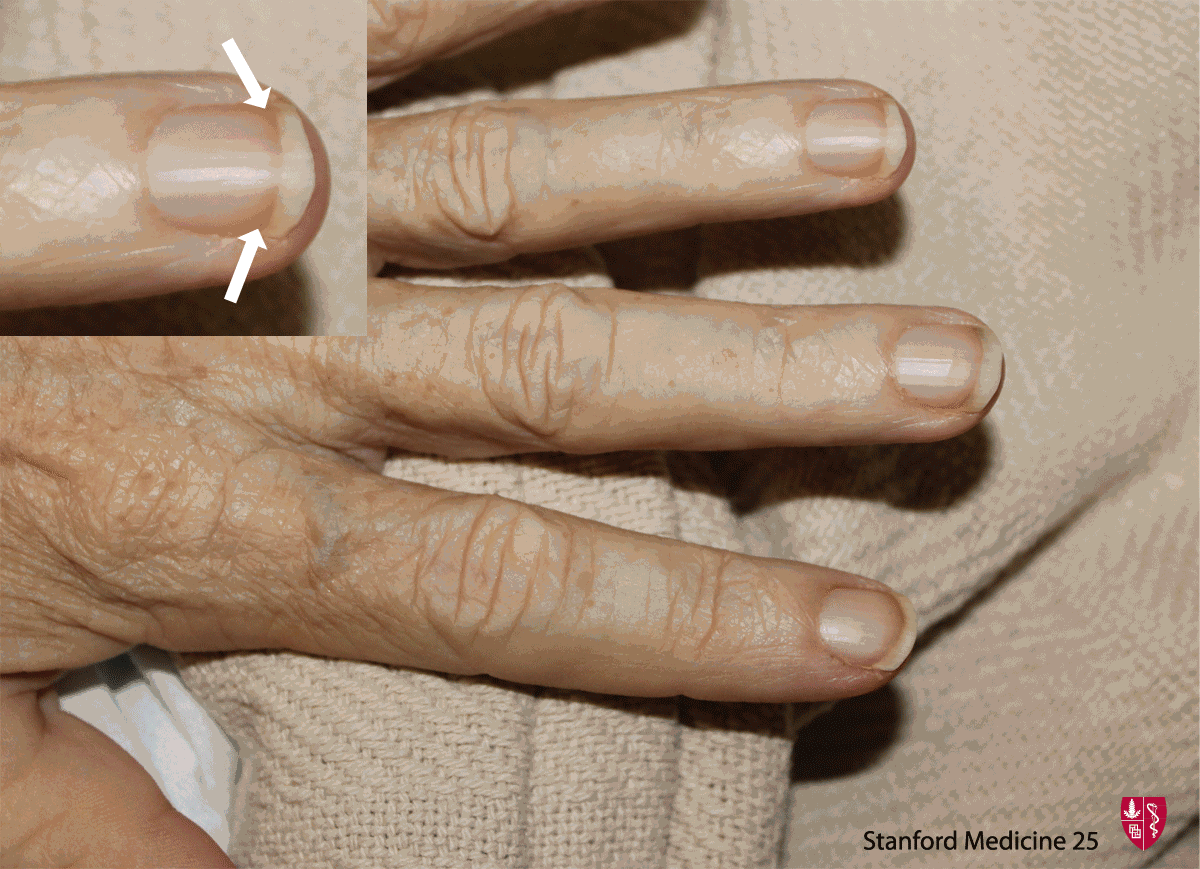
Lindsay’s nails (‘half-and-half nails’)
Distal brown transverse band seen in chronic kidney disease (CKD). Caused by increased pigment deposition.

Mees’ lines
Transverse while lines (usually one per nail, no depressions) that often can will disappear if pressure is placed over the line. It is associated with arsenic, thallium poisoning and other heavy metal poisoning.

Muehrcke’s lines (leukonychia striata)
Narrow while transverse lines (not depressed, compared to Beau’s lines). Usually 2 or more lines on one nail. Seen in states of decreased protein synthesis or increased protein loss, such as with hypo-albuminaemia (usually less than < 20 gL), certain chemotherapy and nephrotic syndrome.

Nail pitting
Non-specific sign for psoriasis (additional signs include onycholysis, thickening, and ‘oilspot’ lesions which are yellow patches on the nail).

Nailfold infarcts
Seen in infective endocarditis and many autoimmune diseases.

Nicotine stained nails
Nicotine stained distally, but not proximally with clear line of demarcation. May also appear when patient switches to ‘lower tar’ tobacco.

Paronychia
Inflammation of the nail folds – red, swollen, often tender. Frequent immersion in water a risk factor for chronic paronychia.

Splinter haemorrhages
Nonspecific finding associated with trauma most commonly but also seen in infective endocarditis and many autoimmune diseases.

Proximal paleness extending halfway up the nail, often eliminating the lunula. Darker distal band. Seen in states of stress (e.g. advanced age, chronic liver disease/cirrhosis, CHF, DM2).
Fingers
Bouchard’s and Heberden’s nodes
Bouchard nodes (found at the PIP) and Heberden’s nodes (found at DIP) are bony outgrowths seen in osteoarthritis of the hand. These outgrowths are formed by calcific spurs within the respective articular joint.

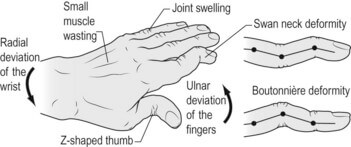
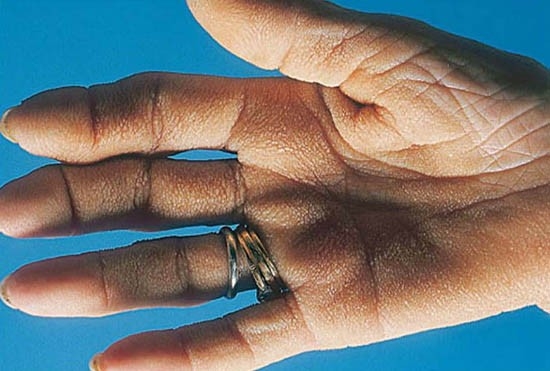
Boutonniere & swan neck deformities
Boutonniere: flexion of PIP, and extension of DIP – seen in chronic rheumatoid arthritis (RA).
Swan neck: extension of IP, flexion of DIP – seen in chronic rheumatoid arthritis.
Herpetic whitlow
Occupational hazard for health professionals who work around oral secretions.

‘Fingerisation’ of Thumb-Holt-Ohram Syndrome
Holt-Ohram syndrome – absent radius, single atrium, autosomal dominant.

Hands
Ape hand
This is a condition in which the thumb is permanently rotated and adducted, resulting in a loss of its opposable function – due to distal median nerve dysfunction.
To show this, ask the patient to use both hands to make and ‘OK’ sign by forming a circle with thumb and index finger. Median nerve palsy may make one hand produce a pinched circle (right hand in image).

Arachnodactyly (achromachia, or ‘spider fingers’)
Long ‘spider-like’ digits, thumb can often extend beyond palm. Characteristic of Marfan’s Syndrome = tall stature, thoracic deformity, joint laxity, ectopia lentis and myopia, aortic dilation and dissection, mitral valve prolapse, autosomal dominant, spontaneous pneumothorax, chordae tendineae rupture.
Claw hand
This is due to ulnar damage, when the 3rd & 4th lumbricals are unable to extend the PIP & DIP joints at the 4th & 5th digits.
Ulnar nerve damage may also cause hypothenar atrophy.

Froment’s signAsk the patient to hold a piece of paper between thumb and index finger. If the examiner can pull paper away (a positive Froment’s sign), it suggests that an ulnar palsy has weakened the thumbs strength of opposition.
Liver disease (chronic)
There are 19 recognised of chronic liver disease in the hands, that can be recognised on a diagnostic handshake (more common ones are in bold).
- Abscesses
- Clubbing (only in biliary cirrhosis; see above)
- Dupuytren’s contracture ..

- Flapping tremor (metabolic flap)
- Jaundice
- Koilonychia (see above)
- Leuconychia (see above)
- Needle marks (Hep B/C?)
- Palmar erythema (pale hands with redness over thenar and hypothenar eminences)
- Pallor
- Porphyria cutanea tarda (PCT)
- Purpura
- Oedema
- Scratchmarks
- Spider naevi (also look for in face and on neck)
- Tattoos (Hep B/C?)
- Tremor (alcohol excess or withdrawal)
- Terry’s ‘half & half’ nails (see above)
- Xanthomata.
Hypermobility of hand joints
Ehlers-Danlos, many types. Syndrome may include skin hyperextensible, fragile, ‘cigarette paper burn’ scars, spontaneous rupture of eye, arteries, intestine, hip dislocations, Marfanoid habitus, kyphoscoliosis, prominent hernia, mitral valve prolapse, coronary dissection.
Pope’s hand (‘Hand of Benediction’)
The Pope’s hand is seen with proximal median nerve dysfunction when asking the patient to make a fist due to inability to flex 1st & 2nd fingers at PIP. Additionally there may be thenar atrophy.

Radial nerve damage
No intrinsic muscles of hand but important wrist extensors. Radial nerve damage commonly causes wrist drop.

Short extremities and polydactyly
Ellis Van Creveld Syndrome – dwarfism, short extremities and polydactyly, dysplastic teeth and nails, multiple frenula binding the upper lip to the alveolar ridge, ASD or a single atrium.

Palms
Down’s syndrome
Single palmar crease (Simian crease). The fifth digit is abnormally short (only reaches the second crease of the 4th digit). Remember to look for endocardial cushion defects (ASD, VSD and mitral/triscuspid abnormalities).

Janeway lesions vs Osler nodes
Both are found in bacterial endocarditis.
Osler nodes. Painful, palpable red lesions usually on fingers/toes. They are caused by immune complexes.

Janeway lesions. Non-painful, macular lesions, usually on palms/soles. They are caused by septic emboli, more common in Staph aureus endocarditis.

Syphilis (secondary)
The characteristic rash of secondary syphilis may appear as rough, red, or reddish brown spots both on the palms of the hands and the bottoms of the feet.

Tripe hand
Thickened, velvety texture of hand. Often sign of visceral malignancy.
Xanthomata
These are raised yellow cholesterol-rich deposits, which can be noted on the palms (and tendons of the wrist and elbow). Xanthomata are associated with hyperlipidaemia.
Xanthomas palmaris




