10 pneumonia facts
In this article we will describe 10 in depth facts about pneumonia, focusing on its symptoms, causes, and treatment.
Key Points
- Pneumonia: is an acute lower respiratory tract infection (LRTI) with new radiological consolidation
- Diagnosis: is based on chest x-ray and clinical findings
- Causes, symptoms, treatment and prognosis: differ widely depending on:
- Bacterial, mycobacterial, viral, fungal, or parasitic
- Acquired in the community (CAP) or hospital (HAP)
- Mechanical ventilation
- If immunocompromised.
- Severity: use CURB-65 score to assess
- Differential diagnosis: includes fluid overload (heart failure or AKI). If in doubt, treat both.
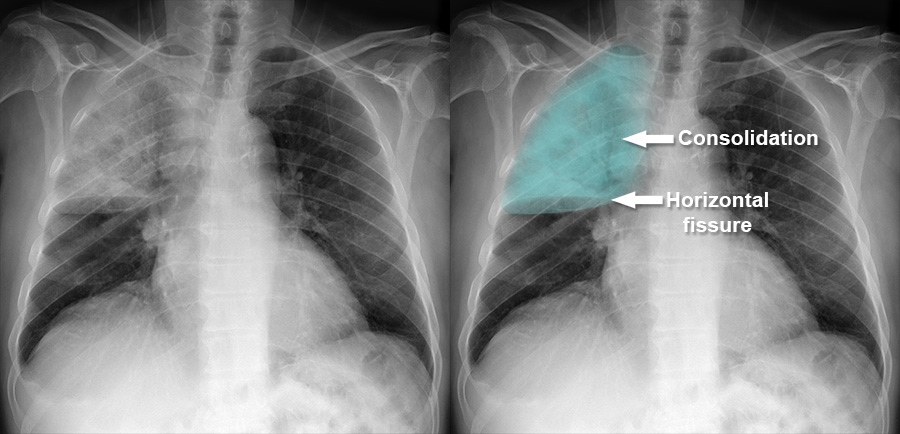
Right upper lobe pneumonia
1. Definition
- Pneumonia is an acute lower respiratory tract infection (LRTI) characterised by new radiological consolidation on a chest x-ray, affecting one or both lungs
- It involves inflammation of the alveoli (air sacs), which fill with pus or fluid
- This leads to symptoms such as coughing (often with yellow-green sputum), fever, rigors, and in some cases, shortness of breath.
Classification
Pneumonia can be classified based on:
- Anatomy: Which part of the lung is affected (e.g. right upper lobe pneumonia).
- Causative agent: Bacterial, viral, fungal, parasitic, or mycobacterial.
- Location of acquisition:
- Community-acquired pneumonia (CAP)
- Hospital-acquired pneumonia (HAP)
- Healthcare-associated pneumonia (HCAP)
- Ventilator-associated pneumonia (VAP).
2. Epidemiology
Pneumonia is more common in young children under five and adults over 75. Individuals with pre-existing health conditions, such as chronic respiratory disease, are at higher risk.
3. Risk factors
- Age – infants, elderly
- Smoking
- Alcohol use
- Pre-existing respiratory conditions – COPD, asthma, lung cancer, bronchiectasis
- IV drug use
- Hospitalisation
- Immunosuppression – e.g. HIV, chemotherapy)
- Other: PPIs, poor oral hygiene?
4. Causes
- Community-acquired pneumonia (CAP): occurs outside hospital; most common pathogens:
- Bacterial: Streptococcus pneumoniae (most common), Haemophilus influenzae, Staphylococcus aureus, Moraxella catarrhalis
- Atypical: Mycoplasma pneumoniae, Chlamydophila pneumoniae, Legionella pneumophila.
- Viral: influenza A/B, SARS-CoV-2, rhinoviruses, parainfluenza, adenoviruses, respiratory syncytial virus (RSV)
- Fungal: Cryptococcus neoformans, candida, Aspergillus, Histoplasma capsulatum, Pneumocystis jirovecii.
- Hospital-acquired pneumonia (HAP): infection after 48 hours of hospital admission; common pathogens: Pseudomonas aeruginosa, Escherichia coli, Klebsiella pneumoniae, Streptococcus pneumoniae, Staphylococcus aureus (including MRSA).
- Ventilator-associated pneumonia: occurs 48-72 hours after tracheal intubation; pathogens similar to HAP.
- Aspiration pneumonia: inhalation of oropharyngeal contents; common in swallowing dysfunction, general anaesthesia (post-op), delayed gastric emptying, poor cough; microbiology similar to non-aspiration pneumonia.
5. Symptoms
- Cough, often with yellow/green sputum and sometimes haemoptysis
- Pleuritic chest pain (worse with breathing, movement, and coughing)
- Fever and rigors
- Shortness of breath
- Fatigue and muscle aches.
In severe cases, older adults may present with acute confusion.
Onset
Pneumonia can develop quickly (over 4-6 hours). It usually develops more gradually over a few days. Some patients may initially present with acute chest pain.
6. Diagnosis
Pneumonia is diagnosed through a combination of clinical assessment and investigations:
- Chest x-ray: Essential for diagnosis, showing consolidation
- CT scan or bronchoscopy: May be needed to identify specific causes
- Blood tests: Including arterial blood gas (ABG)
- Urine tests: Legionella and pneumococcal urinary antigen
- Blood cultures and sputum cultures: To identify pathogens.
Calculate CURB-65 score:
- Confusion, Urea >7 mmol/L, Respiratory rate ≥30, Blood pressure <90 systolic or ≤60 diastolic, Age ≥65.
- Score 0-1: low risk (outpatient treatment).
- Score 2: moderate risk (consider inpatient or supervised outpatient treatment).
- Score 3-5: high risk (inpatient treatment, consider critical care).
Differential diagnoses
- Pulmonary embolism (PE)
- Acute heart failure
- Pleuritis/pericarditis
- Pneumothorax
- Other respiratory infections.
7. Treatment
Treatment varies depending on the underlying cause:
- Bacterial pneumonia: Treated with antibiotics (oral or IV).
- Viral pneumonia: Usually managed with supportive care, but antivirals may be required in certain cases.
- Fungal pneumonia: Requires antifungal medications.
Supportive care includes rest, fluids, and antipyretics/analgesics (e.g. paracetamol, NSAIDs). Mild cases can be managed at home with regular monitoring, while severe cases may require hospitalisation.
8. Complications
- Pleural effusion: Fluid accumulation around the lungs
- Empyema/lung abscess
- Sepsis: potentially life-threatening complication
- ARDS
- Post-infective bronchiectasis.
9. Prognosis
- Recovery from pneumonia typically takes 2 to 4 weeks, but full recovery may take up to 3 months in more severe cases
- The 30-day mortality rate for hospitalised patients is around 15%, rising to 30% in patients over 85 or those in intensive care
- Patients with HAP, those on mechanical ventilation, and immunocompromised individuals have a worse prognosis.
10. Prevention
- Vaccination
- Pneumococcal (PPV, PCV) – for infants, elderly, and at-risk groups
- Haemophilus influenzae type b (Hib) – as part of childhood immunisation schedule
- Lifestyle measures: Good hygiene practices, smoking cessation, and avoiding close contact with sick individuals can reduce the risk of pneumonia.
Summary
We have described 10 in depth facts about pneumonia, and its symptoms, causes, and treatment. We hope it has been helpful.
Top Tip – Pneumonia
If a patient with severe pneumonia is unwell, and the microbiological cause is unclear, treat with IV broad spectrum antibiotics, antivirals, antifungals and antiprotozoa drugs. Get a infectious disease or clinical microbiology opinion soon.

