Respiratory medical history taking
We will now describe respiratory medical history taking. As with all medical history taking ..
Listen to your patient, he is telling you the diagnosis”. Dr William Osler (1849-1919)
.. and 90% of the diagnosis is in the medical history. Full stop.
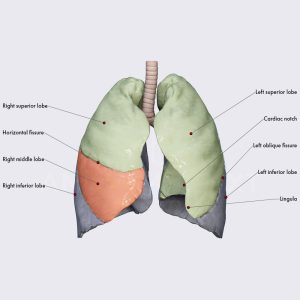
Lung anatomy is different on the right and left. Most of the posterior chest wall is over the lower lobe.
It is important to ask questions about all of the respiratory system, including the symptoms of heart failure (cor pulmonale). These questions can be used in a clinical or examination setting.
Pre-introduction observation (before questions)
Before you start, stop, slow down and think. Just for 15 seconds.
Right. Antennae up. Observe the patient and environs around the patient. Why?
Observation is 90% of medicine”
What can you see? What’s their biological age? Walking pace? How are they dressed (and why)? What are they reading (and why)? Are they in pain (from where)? What’s their mood? Are they short of breath or have ankle swelling (fluid overloaded)? Coughing? Dizzy and maybe falling (low BP? dry?)?
Wash hands. Now you can ask questions. Clock on. Here we go ..
How to take a respiratory medical history
These are ten questions you can ask, and the words to use. They can be asked in ten minutes.
1. Introduction – Start with a diagnostic handshake. “Hello, my name is XX and I’m a student doctor YY. You are Mr/Mrs ZZ and you are AA years old. Is that correct?” You can ask date of birth but that takes longer and you have to do mental arithmetic to calculate the age. The handshake is also a diagnostic tool.
2. PC – “What is the current problem?” Listen very (very) carefully. The diagnosis is often in the patient’s first few words. Write it down. Come back to that at the end.
3. HPC – “Please tell me more about the problem”. Ditto.
Most respiratory symptoms are not especially specific to respiratory disease, e.g. chest pain on inspiration, coughing, moving and sitting forward (pleuritic), are the same features of pericarditic pain. A sudden onset of pleuritic chest pain suggests pneumothorax.
Alternatively symptoms may be very non-specific, as there are other (non-respiratory) causes, e.g. fatigue, collapse, shortness of breath (SOB) or ankle swelling.
To save time, ask relevant questions from systems review here. These include questions about cough, haemoptysis, calf swelling and tenderness (DVT?). You will not have time to do a full systems review.
4. PSH – “What major operations have you had?”. You are especially interested in lung surgery (e.g. for cancer or COPD).
5. PMH – “Have you ever had .. diabetes, jaundice, anaemia, tuberculosis, heart attacks, strokes, high blood pressure, epilepsy, rheumatic fever, or ulcers in your tummy?”
Specific respiratory questions include: “have you ever had childhood chest infections (bronchiectasis), lung cancer, lung fibrosis, COPD, or a PE/DVT?”
You need to have finished PMH by 5 mins
6. Drugs/Allergies – “Please show me a list of your current medication? And have you had a major allergic reaction to any medication?”
The medication history is important in respiratory disease, e.g. drug causes of pulmonary fibrosis (such as amiodarone). You need to take it carefully. Ask about inhalers.
7. SH – “Are you married, how many children have you had, and what is/was your current/last job?”
Occupation and hobbies are very relevant for respiratory disease. You should ask about current and all previous jobs. You are looking for exposure to asbestos, coal and other substances.
You are looking for the pneumoconioses, e.g. asbestosis (caused by inhaling asbestos fibres), silicosis (silica dust), and Coal workers’ pneumoconiosis (coal dust).
Do they keep budgerigars (Bird Fancier’s Lung)?
8. SH – “Have you ever smoked, and have you ever been a regular heavy drinker?”
Smoking is the primary risk factor for lung cancer and COPD.
9. FH – (depending on age of patient) “Are your parents alive fit and well? OR “Are your parents still with us?” Depending on answer, “what did they die of?” OR “What did your parents die of?” AND “Are there any diseases that run in the family?”
“Has anyone in your family ever had COPD or a long-term lung condition ” (e.g. alpha-1 antitrypsin deficiency)
“Has anyone in your family had any funny or rare diseases?” (autoimmune, e.g. SLE, RA, pulmonary fibrosis; or Marfans associated pneumothorax)
You need to have finished SH/FH by 8 mins, to give time for ..
10. ICE – “What are your ideas about what’s going on, and what are your concerns and expectations (of us)?” This also gives time for you to think what have you forgotten .. did you ask about medication/allergies and/or smoking/alcohol?
At this point, the patient may give you crucial information like they have COPD, lung cancer or fibrosis; if it has not come out on previous questioning.
Summary
We have described respiratory medical history taking. The occupational and hobby history is important. We hope you have found it useful. Like all history taking, the only way to get good at it, is to practice alot (alot).

