Uterine fibroids: 10 Q&As (including controversies)
1. What are uterine fibroids?
- Uterine fibroids, also known as uterine leiomyomas, are benign (non-cancerous) growths that develop in the uterus (womb).
- They are made up of muscle and fibrous tissue and can vary in size, shape, and location – they may be tiny or as big as a football.
- Natural history: they often regress (go away) with no treatment, e.g. after a pregnancy or menopause. This facts affects many treatment decisions.
Note. Even though we know this, we don’t know the cause, why they get worse, and why some regress (go away). See below.
2. Who gets fibroids?
- Most women
- Fibroids are very, very common – affecting 70-80% women over 50 years (and Black women have an increased risk).
- And as (normal variant) heavy periods are also very common, there is huge overlap between the two – leading to confusion on whether the fibroids are causing the patients symptoms.
- In fact, the high prevalence means fibroids in most women are actually normal, and do not cause symptoms – i.e. questioning whether they are a disease.
3. Is the diagnosis of fibroids easy?
Yes/no.
It is easy to do a scan (e.g. an ultrasound or MRI) and diagnose fibroids (with a degree of certainty). This does not mean:
- They are the cause of the symptoms.
- Treatment is required or will work (see below).
Why?
- There is difficulty distinguishing fibroids from other conditions: (e.g. adenomyosis, endometriosis) due to overlapping symptoms and imaging limitations.
- Non-specific symptoms: Fibroid symptoms overlap with (normal variant) heavy menstrual bleeding, and other conditions, making diagnosis difficult.
- Variability in presentation: Fibroids can be asymptomatic or cause severe symptoms.
And are the investigations reliable?
Yes, but .. ultrasound (and MRI) may not always accurately diagnose or measure fibroid size/location.
4. Does the treatment work? (and which is ‘best’)
Yes, but ..
Multiple treatments exist (medical, surgical, minimally invasive), but there is no single ‘best’ approach, leading to confusion and inconsistent outcomes. Also different specialists favour different treatments. Some will ‘push’ surgery; others will do the opposite.
5. What is the natural history of fibroids?
- Many regress (‘go away’) eventually – especially after pregnancy or the menopause.
- This is a big part of the problem with the management/treatment of fibroids (and how common they are)
- So, doing nothing may be the best option.
6. Do we know what causes them, and causes them to grow or regress (go away)?
No. This a major problem.
- There is uncertainty about factors affecting fibroid growth, regression, and impact on fertility and pregnancy complicates treatment decisions.
7. Are patients educated about fibroids and aware of all options?
No. Another problem.
- Patients often lack understanding of fibroids, treatment options, and potential outcomes, hindering informed decision-making. Also many people dont like talking about menstrual periods, delaying diagnosis and treatment.
8. Is there easy (and equal) access to NHS specialist care?
No.
- There is limited access to experts in fibroid management, particularly for less advantaged populations – with long waiting lists for treatment (including surgery) in the NHS.
- Lack of standardised guidelines: So, when you do see someone, they may not agree with a similar specialist (and hence you will get quite different care from two similar doctors).
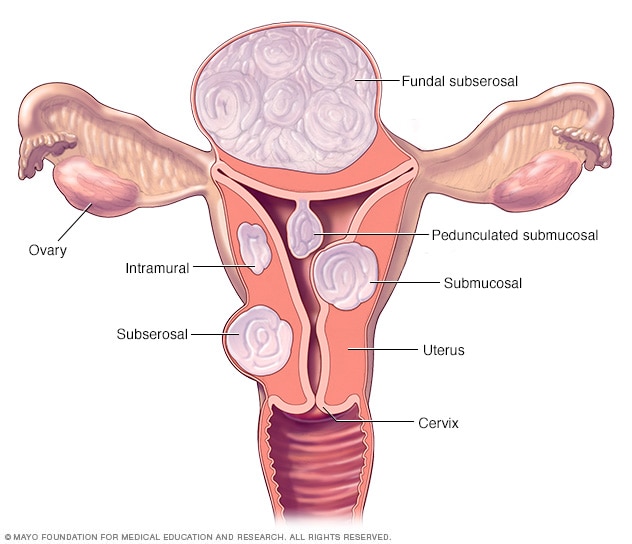 Different types of fibroid
Different types of fibroid9. What more research needs to be done?
-
Pathophysiology: Understanding fibroid development and growth.
-
Effective medical therapies: Developing targeted treatments.
-
Minimally invasive techniques: Improving surgical outcomes.
-
Fibroid-specific quality of life measures: Developing standardised assessment tools.
-
Long-term outcomes: Studying treatment effectiveness and recurrence rates.
10. What are the main challenges that need to be addressed in the long-term?
-
Improved diagnostic tools and techniques.
-
Standardised treatment guidelines.
-
Enhanced patient education and awareness.
-
Increased access to specialist care.
-
Better research regarding fibroid biology, and which is/are the best treatment option(s).

