What is good (and less good) about the NHS?
We put the question “what is good (and less good) about the NHS?” to a group of mainly non-medical friends. This page summarises their answers, including some quotes from them.
Remember as we are ‘on the inside’. So we are of course harsh critics. We want it to be excellent or at least very good every day. What is more important is your view on how good or less good it is. Please contact us with your views. We would love to hear them. Here goes with their view. We have added some explanation to what they think.
What is good about the NHS?
1. One organisation that provides universal care, free at the point of use
- The NHS was founded on the principle of universal healthcare, free at the point of use. This principle of comprehensive health care based on clinical need rather than the ability to pay is vital in a fair society. This point is as valid now as it was in 1948 when the NHS started
- The NHS leads (or led!) the world in terms of equity of access and ensuring people don’t suffer financial hardship when they are ill. Other nations have caught up and are providing better healthcare now. Just because you ‘invent’ football, doesn’t give you the right to be good at it
- As it is one organisation, different parts of it work well together (or try to). For example there are ‘networks’ of hospitals that organise the transfer of patients from smaller to larger (more specialised) hospitals and back. Staff try to help each other in other places
- A financial system called ‘specialised commissioning’ means rare and expensive diseases are paid for, so you are not disadvantaged if you are unlucky and have such a disease.


2. Primary care, especially general practice (GP) and pharmacy
The traditional form of General Practice (GP) still exists in the UK and (by and large) works well. All of us are registered with a GP, who is responsible for our long term physical and mental healthcare, and liaising with hospital consultants. This is not true of all countries.
Also, some primary care services – e.g ‘first contact’ physiotherapists and counsellors (called ‘IAPTs’) – are now available without GP referral. So you can refer yourself for these services. That pharmacies are part of the NHS (and there is usually one near to your GP, working with them) is another major plus point.
3. Some ‘out of hours’ healthcare
Some parts of the NHS – including A&E, NHS111 (telephone and cyber advice service), coronary and intensive care (adult and neonatal), labour ward, emergency surgery – function 24 hours a day, 7 days a week. Walk-in/Urgent Treatment/Minor Illness/Injury centres are open 8am-8pm, 7 days a week.
4. Employment
The NHS employs 1.5 million people, making it the biggest employer in the UK and Europe, and 5th biggest in the world. This is ‘good’ in some ways. It is part of the reason that there is a strong emotional bond between the public and the NHS, as we all know someone in it – as well as needing and using it.
The NHS is still a ‘good’ employer, with better than average pensions and working conditions, such as maternity, and annual and study, leave – and clear career progression.

But its size is also an issue. Perhaps it is too big, and this is part of the reason its performance is not great at present (see point 7 below). Healthcare is devolved to the 3 nations of the UK. This is helpful. But is the NHS in England too big, and should it be split up into several regional health services (like the ‘state system’ in Australia)? Could it be run by the council, like social care? What do you think?
5. Education, regulation, and standards
As the NHS has been running for over 70 years, there has been time to develop bodies that support and help it; and provide independent constructive criticism and challenge. Examples include:
- Health Education England (HEE)
- Makes it easy to get funding and time for postgraduate courses and exams
- Develop new health professions, e.g Physician Associates (PAs), Advanced Clinical Practitioners (ACPs). Advanced Nurse Practitioners (ANPs), Allied Health Professionals (AHPs)
- Can change the function of professions, e.g. paramedics doing home visits for GPs
- Royal Colleges and other professional bodies – set exams, keep up standards and inspect underperforming units
- General Medical Council (GMC; the doctors’ regulator) and other regulators
- Care Quality Commission (CQC; inspector)
- National Institute of Health and Social Care Excellence (NICE) – publishes guidelines on what treatments (including drugs) are cost-effective and can be used.

6. Drug industry
This works well with the NHS, NICE, and a regulatory body called Medicines and Healthcare products Regulatory Agency (MHRA).
7. Good value for money
The NHS is well funded as this is linked to population growth. Most government ministries do not have that advantage.
However there is no legal requirement to stay in financial balance. This is an issue. It encourages over-spending and poor accounting as purchasers (like NHS England) and providers (e.g. hospitals) are allowed to be bankrupt; thus avoiding hard decisions on what NHS services should or should not be provided. It also allows – and indeed may encourage – the NHS to do (for example) 10 things badly, rather than 5 things well.
It costs about 10% of your taxes (GDP), and about £2700 per person per year. This makes it good value, and comparable to other developed countries.
OK OK. It cannot be all good. Tell us .. what do you (really!) think of the NHS?
What is less good about the NHS?
1. Primary care, especially GP. How can it be good and bad? Well, it is true. It is currently hard to get face-to-face appointments, which many of the public (especially older ones) prefer. There is lack of continuity as practices close and merge; making it very hard to see the same GP twice. The appointments (8 mins) are far too short as well.
2. Mental healthcare, especially childrens’ (CAHMS)
There is nowhere near enough provision for the tsunami of patients with mental mental health problems. The excuses are over.
3. Elective (e.g. a planned operation) and non-elective (emergency) care
These occur in the same hospital. This means that planned operations are constantly cancelled or postponed due to emergency admissions, who compete for the beds. These latter patients are the fail elderly like our/your grandparents, who also deserve the bed. It is a primary cause of poor performance, see point 7 below).
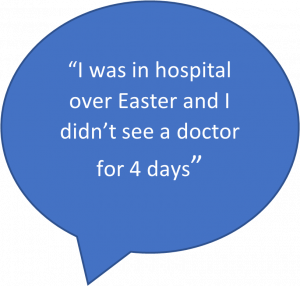
4. Lack of a 7 day service (7DS), and most ‘out of hours’ healthcare
Society now expects most aspects of society to work 7 days a week. Amazon, Ebay, Tescos, Booking.com and Premier Inn work at weekends and bank holidays. The police provide a 7DS, often putting more staff on at night and at weekends, as the need is greatest then. Most of the NHS does not. The excuses are over in this area as well. Doctors have resisted modernisation in the past, and in this area now. Ditto re point 7.
Note. It is also wasteful of money, as operating theatres etc are hardly used at weekends but still have to be heated and cleaned etc.
5. Poor information technology (IT)
Hospital, GP, mental health, pharmacy, and ambulance computers do not link up. They could do. Neither does one hospital link to the next one. There is no national NHS IT system. All of this is technically possible. Sub-regional combined computer systems called EPRs (electronic patient records) are coming in, but slowly. It is a factor in point 7 as well. The NHS website and app are good though.
6. Poor organisation (including links to Public Health, and confusing names)
There is little overlap (and not much co-operation) between:
- Health and social care. They are intrinsically linked but social care is poorly funded. Different government departments are responsible
- Regional substructures – e.g. the regions of NHS England, ambulances, HEE, and Public Health (United Kingdom Health Security Agency, UKHSA) are different in number and geography. All have different email and IT systems, funding streams, and ambitions. This is part of the reason why our performance against COVID-19 was so poor (despite a good vaccination programme)
- Both are factors in point 7 as well.
There are also multiple names for similar parts of the NHS, e.g. Walk-in and Urgent Treatment Centres and Minor Illness/Injury Units. So the public get confused and do not know where to go.
7. Performance
This is the Achilles heel of the NHS. Both:
- Quantity/targets. Hospital performance against the key NHS targets is poor, very. This includes the main ones: 4-hour A&E, 18-week outpatient referral and treatment, and 2-week cancer targets. Waiting lists are now far too long, with over 7 million people waiting for operations. Some people wait over two years for surgery or a procedure. All of this is especially true for the commoner diseases, e.g. those of the hips, knees, eyes and skin
- Quality. The NHS lags behind in saving lives when treating many of the leading causes of death including several types of cancer, heart attacks and stroke.
Summary
We hope that this page summarises what is good and less good about the NHS. But we would really like to know YOUR view. What do you think of the NHS?

